+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you an under-graduate, in College, Bachelors or under-taking your Post graduate studies and need someone to help write your essay or research? We offer premium quality essay writing help. All our papers are original, 0% plagiarized & uniquely written by our dedicated Masters specialists. My Essay Services is an experienced service with over 9 years experience in research writing of over 97,000 essays over the years. You will receive a plagiarism check certificate that confirms originality for any essay you order with My Essay Services. Fill the calculator on your right to begin placing your order now!
Are you an under-graduate, in College, Bachelors or under-taking your Post graduate studies and need someone to help write your essay or research? We offer premium quality essay writing help. All our papers are original, 0% plagiarized & uniquely written by our dedicated Masters specialists. My Essay Services is an experienced service with over 9 years experience in research writing of over 97,000 essays over the years. You will receive a plagiarism check certificate that confirms originality for any essay you order with My Essay Services. Fill the calculator on your right to begin placing your order now!

Abstract
 Understanding the cultural context of illness is extremely important for diagnostic assessment and clinical management (Robert Hogan, 1997). This is because there is nobody that exists oblivious of culture. Therefore, in order to make the correct diagnostic assessment as well as clinical management culture is a big factor that should play.
Understanding the cultural context of illness is extremely important for diagnostic assessment and clinical management (Robert Hogan, 1997). This is because there is nobody that exists oblivious of culture. Therefore, in order to make the correct diagnostic assessment as well as clinical management culture is a big factor that should play.
It is of the essence to understand that cultures are open and dynamic systems that often undergo continuous change over time. The cultural factors that one should look at in making a culturally diagnosis such as that of ‘Andrea C’ firstly is the perception of the community towards mental health. It is important to ensure that the persons are not victimized and the psychologist should go to lengths to ensure that this does not happen (Pomerantz, 2008). There is a need to protect the integrity of the patient and his livelihood.
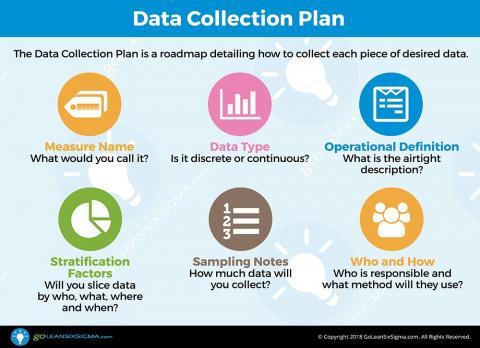
Read more on qualitative and quantitative data collection
Secondly, another factor that should be looked at is cultural identity of the individual, and the reference groups that might in one way or another influence his or her relationships with other persons. There is also a need to look at some taboos that exist in the culture and how one can be able to ensure that he gives proper psychological attention to the client while at the same time respecting the culture of the person (Yael Latzer, 2011). For this reason, it is important for the psychologist to understand the schematics that are involved when it comes the patient’s culture, the dos and the don’ts. This will be of the essence in ensuring that the psychologist understands the importance of culture in the proper diagnosis as well as treatment of an individual. The culturally sensitive diagnosis ensures that clients such as ‘Andrea C’ are well understood.
References
Pomerantz, A. (2008). Clinical psychology : science, practice, and culture. Los Angeles: SAGE.
Robert Hogan, J. J. (1997). Handbook of personality psychology. New York: McGraw Hill.
Yael Latzer, J. M. (2011). Understanding eating disorders : integrating culture, psychology and biology. New York: SAGE.
In the current world, nursing is one of the major careers as it deals with healthcare. Nursing practice has become more demanding over the past years due to increasing patients demands and public expectations. This has led to massive changes in nursing education to enable nurses perform better. Research utilization and Evidence- Based Practice(EBP) are some of the major nursing practices.
Research utilization entails thorough clinical research on nursing practices. Therefore, in research utilization knowledge is only acquired through researches. However, in Evidence- Based Practice, there is more than research required. The practice involves using patients preferences and values together with research in order to provide the best quality care. Thus, research utilization is part of evidence-based practice.
In my internship at a local hospital, I was required to sort some clinical questions through numerous consultations. First, I was obliged to inquire the patient’s preferences and values. Second, I was required to gather the best evidence regarding the clinical problem. Third, I engaged in numerous consultations with doctors and the head nurse on the best practice. Finally, I integrated all the evidence and after assessing the best practice, considering resources available in the hospital, I settled for the most appropriate clinical decision. This enabled me to enhance my clinical practice experience to achieve the best patient care. Therefore, internship roles play a major role in improving education research understanding of patient care.
Besides graduate education, clinical practitioners should engage in other practices such as understanding patient values. This will help improve the current nursing potential. Most countries have settled for the evidence-based practice as the most ideal nursing practice.
References
Hamric, A. (2009). Advanced Practice Nursing (4th ed). W.B. Saunders Company
 Although many may think evidence base practice (EBP) and research are the same they are entities of their own. EBP is a term devised at a medical school in Canada to describe a teaching-learning strategy designed to shape clinical decision making specifically in medicine. Research is the gathering and generating of new information about a phenomenon or validating an existing one. EBP is used to validate our research, there are three primary factors: best research evidence, applied with clinical expertise, and applied with an appreciation of the patient’s values and expectations. As APN we think of ways that could prove better outcomes for our patients using our clinical experiences, that’s the critical thinking part.
Although many may think evidence base practice (EBP) and research are the same they are entities of their own. EBP is a term devised at a medical school in Canada to describe a teaching-learning strategy designed to shape clinical decision making specifically in medicine. Research is the gathering and generating of new information about a phenomenon or validating an existing one. EBP is used to validate our research, there are three primary factors: best research evidence, applied with clinical expertise, and applied with an appreciation of the patient’s values and expectations. As APN we think of ways that could prove better outcomes for our patients using our clinical experiences, that’s the critical thinking part.
Then, we collect the data through published research. Once the question is born and the research is collected we put them together to evaluate the result. There are three different steps in putting this together. First, we must ask ‘why’: synthesize the evidence. Next we evaluate the practice, this consisting of three competencies: I: integration and use of research and other EBP decision making; II: evaluate the practice; III: participation in collaborative research. Last, is the summary and conclusion: was the question answered and was it supported with research and clinical evidence? (Hamric, Spross, & Hanson, 2008, p. 232).
In the ICU, at the hospital I work for, we are diligent about keeping track of ventilator acquired pneumonia (VAP). VAP can develop approximately 48 hours after intubation. The lungs are sterile and when we insert a tube to help a patient breath there is always a chance that an organism can invade the lower respiratory track; thus causing pneumonia. (Sedwick, Lance-Smith, Reeder & Nardi, 2012) The lungs can also be compromised from gastric or oral secretions because of aspiration during intubation. Our last recorded VAP is March 8, 2007. We pride ourselves in providing oral/mouth care every 4 hours and PRN (as needed). EBP has proven that oral care given to ventilator patients every 4 hours is at a 95% decreased risk of VAP. (Sedwick, Lance-Smith, Reeder & Nardi, 2012) There are other areas in which EBP is utilized in our hospital like many others; such as blood stream infection, urinary tract infection, and congestive heart failure. The core measure policy was activated because of EBP and the best outcome for the patient.
Research and EBP are a large part of the master’s education level. We are designed to try and make things better, and EBP allows us to do that. I would actually like to conduct a study on ICU psychosis. The stay for the patients I care for is usually between 3-5 days. I have witnessed mental changes in some of these patients that seemed to have cleared once a number of constants changed. I am also a firm believer in a good bath and back rub, not just for ICU patients but anyone who is considered total care. I think this stems back from the first semester in nursing school when my professor spoke about holistic care.
Currently, the bed/bath team uses ready-made wipes and only takes about 15 mins per patient. I know times are changing and hospitals and other healthcare facilities are trying to cut cost, but I’m not sure it should be in this area. I believe with technology as advanced as it is and a higher level of education, such as a master’s degree, put together is a recipe for a greater tomorrow. We must now provide evidence base practice for the upcoming nurses just as seniors nurses have provided for us.
Research involves the gathering of information pertaining to specific subjects within the healthcare field, with the goal of integrating findings into practice or evaluating the current standard of practice to determine if better methods are needed. Evidence based practice builds off of research and certainly incorporates it as part of the problem solving process. Hacket et al. provides a definition of Evidence Based Practice that incorporates three separate criteria; 1) best research evidence, 2) applied with clinical expertise, 3) applied with an appreciation of the patient’s values and expectations (Hamric, Spross, & Hanson, 2008, p. 221). Evidence Based Practice seeks to takes the specifics of research, and incorporate a more holistic view of them by working in conjunction with a nurses own experiences as well as patient preference.
In my own department, the Cardiac Cath Lab, we use a very large quantity of anticoagulant and anti platelet medication on our patients, specifically patients who undergo primary PCI (angioplasty/stent placement). With such a heavy emphasis placed on the use of anticoagulants, and the overall invasiveness of the procedure we perform, we place a strong concern on bleeding complications. We keep track of closure device failure, hematoma formation, retroperitoneal bleeding, as well as gross bleeding from the puncture site. These bleeding complications are monitored for as long as 30 days post procedure. Any CCU or Cardiac PCU nurse knows how seriously we take these complications. The mainstay of treatment for these procedures in the past has been the use of UF Heparin, but within the last decade a new drug called Angiomax (Bivalirudin) has been implemented in some cases.
Recently I led an evidence based practice project in my department evaluating which of these two forms of anticoagulation were associated with fewer bleeding complications for the patient. We found research in the form of the HORIZINS AMI trial, which showed complications to be significantly fewer having received Angiomax over Heparin. Instances of minor bleeding, major bleeding, post procedure blood transfusions, and in stent restenosis rates were all lower having used Angiomax over Heparin (Curran, 2008) As a department we had this discussion with the cardiologists, and with exception to cases where quick reversal of anticoagulation would be needed using Protamine, Angiomax would be our primary method. Throughout the hospital our results have been successful, being largely reflective of the study we used as evidence. Only in a few, very specific cases, do we now use UF Heparin.
Advanced Practice nurses “possess the necessary clinical expertise and have an awareness of patient, family, and health care provider needs” (Hamric, Spross, & Hanson, 2008, p. 222) which help to play a valuable role in the implementation of evidence based practice. I very much hope to play a part in the synthesis and implementation of these practices. Because my goal is to return to the Emergency Department, I would be very interested to see studies related to improving stable patient turnover. This is a significant problem in many Emergency Departments, including my own, due to the use of ED's as primary care offices by a large number of the uninsured population. From the practitioner’s standpoint I would be very interested in researching and implementing methods of streamlining non-urgent patient care to increase efficiency while maintaining quality care. As an Advance Practice Nurse in the Nurse Practitioner role, I one day hope to have this opportunity.
Research and evidence-based practice has been widely used by advanced practice nurses in order to find better ways to take better care of their patients. Research-based practice is a more systematic, rigorous, and precise way of translating research findings into practice (Hamric, Spross, & Hanson, 2009, p. 142). This research is developed and can be used as a standard of care for a population of patients (Hamric, et. al, 2009). Research based practiced involves three steps: (1) locating, evaluating, and summarizing the science; (2) translating the science into clinical recommendations; and (3) strategically implementing the recommendations (Hamric, et. al, 2009 p. 142). These steps allow this type of research to be widely used for the care of many patients.
Research gives advanced practice nurses a baseline of where to start when taking care of their patients with certain issues. Evidence-based practice is practice that involves clinical expertise and patient values (Hamric, et. al, 2009). Evidence-based practice is a more condensed research about certain care involving patients, compared to research practice being broader. Evidence-based research can be used along with research practice by advanced practice nurses when trying to care for patients with specific problems. It gives the nurse an expert opinion, along with abundant research data so the nurse has many views to choose from until she decides which care would be best on that specific patient.
As a critical care nurse, pressure ulcers are an issue that takes priority in the work setting. With unstable patients, skin care can be overshadowed by airway, breathing, and circulation (Flike, 2013). Over the years, research has shown that with adequate nutrition, turning patients every two hours, and keeping patients as dry as possible pressure ulcers can be prevented. In my critical care department we have a protocol that is called Save Our Skin (SOS). With every patient that is admitted, if their Braden Scale is eighteen or less, then that patient is automatically placed on SOS precautions to help prevent or minimize further skin breakdown. This tool is an easy way to remind the nurses that this patient has fragile skin and saving that skin is important. I could take advantage of this opportunity in my graduate role by doing more research about pressure ulcers and prevention methods and introducing this new information to my charge nurses and colleagues. With this new information nurses become more educated and patients are less likely to have skin breakdown.
Research is the gathering of information or evidence to gain knowledge or a further understanding of a particular topic. There are many different types and methods for conducting research. Evidence based practice is a total process that involves knowing how to find the best evidence that is most applicable to a particular healthcare situation, integrating the findings into practice and evaluating the effectiveness of the practice (Hamric, Spross, & Hanson (2009).
In the Medical ICU setting where I work, sepsis is a common diagnosis among patients. Not every patient comes in with it as their primary diagnosis, sometimes it develops during the course of their stay. In an attempt to eradicate sepsis, or at least decrease its occurrence within patients, a committee has been formed on the unit to evaluate the effectiveness of identifying and treating sepsis. Using the “Surviving Sepsis” campaign guidelines, we are looking to see if sepsis is being identified and if the proper treatment, such as administering fluid boluses, retrieving and sending cultures, starting antibiotics, is being done in a timely manner. We hope to develop a protocol that will improve our effectiveness in assessing, identifying, diagnosing and treating sepsis.
In my graduate role I will always make every effort to ensure that I remain proficient with my research skills and ability to recognize useful evidence. I will also continue to assist in implementing evidence into practice as I have already begun to do on the sepsis committee.
References
Hamric, A., Spross, J., & Hanson, C. (2008). Advanced practice nursing: An integrative approach. (4th ed.). St. Louis, MO: SAUNDERS ELSEVIER.
Curran M. Bivalirudin: in patients with ST-segment elevation myocardial infarction. Drugs [serial online].
Flike, K., M.S.N., R.N. (2013). Pressure ulcer prevention in the intensive care unit: A case study. Critical Care Nursing Quarterly, 36(4), 415.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
