+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help write your essay? All you need is to ask for research paper help written by a specialist in your academic field. When you buy an essay online from us, we offer you an original, nil plagiarized and unique paper written by a dedicated writer who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.
Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help write your essay? All you need is to ask for research paper help written by a specialist in your academic field. When you buy an essay online from us, we offer you an original, nil plagiarized and unique paper written by a dedicated writer who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.

 Client Complains
Client Complains
The patient complains about hot flashes and nausea. She explains that the condition started few months ago. She has previously tried natural remedies, but it never worked out.
History of Present Illness
The patient had her last menstrual period one and a half years ago. She experienced irregular periods before they stopped completely. This shows that the patient is experiencing menopause symptoms.
Past Medical History
The patient has been previously diagnosed with Hyperlipidemia five years ago. Further, the patient was diagnosed with gastro-esophageal reflux disease (GERD) two years ago.
Family History
The patient’s mother died from injuries resulting from an accident. On the other hand, her father died of a presumed heart disease in his fifties. She has four sisters and she is the eldest. All of her sisters are alive and well. consequently, the family has no history of breast cancer.
Social history
The patient is married with three adult children who are in good health. She is a part-time bank teller. She walks on her treadmill daily and she watches her grandchildren after school during the week. The patient denies substance abuse, but she admits that she used to smoke two and a half packs of cigarettes per day. However, this was when she was aged fifteen up to forty-five. She drinks alcohol occasionally and ten to twelve diet cokes per day. The patient has tried following a strict low-salt and low-cholesterol diet, but she confessed it has been difficult. Moreover, she has increased her intake of calcium-containing food up to three-four times a day because she does not like taking so many tums.
Physical Assessments Findings
Vital Signs: BP: 130/85 mmHg; P: 85; RR: 16; T : 98.8 oF; Wt : 130 lb ; Ht : 5'8"
GU/Rect: Pelvic exam with pain and mucosal atrophy
Neuro: Within normal limits (WNL)
Cardiovascular: WNL
Skin: Dry and itchy
Lab Tests Findings
Tests Observed Values
Glucose (Glu) 110 mg/dL
Total Cholesterol (TC) 240 mg/dL
High density lipids (HDL) 37 mg/dL
Triglycerides (TRG) 250 mg/dL
Low density lipids (LDL) 160 mg/dL
Thyroid stimulating hormone (TSH) 3.49uIU/mL
Follicle stimulating hormone (FSH) 38 mIU/mL
Luteinizing hormone (LH) 38 mIU/mL
Estradiol level 15 pg/mL
Other tests:
Pap smear and mammogram normal
Negative pregnancy test
Dual energy X-ray absorptiometry (DEXA) scan of lumbar spine and right femoral neck shows slight osteopenia (T scores of minus 1.6, and minus 2.4 respectfully)
Current Medications
Acetaminophen 325 mg 1–2 po qd prn for joint pain after exercise
Prilosec 20 mg bid
Review of Symptoms
Genitourinary/Rectal (GU/Rect): Case of dryness, itching, urinary frequency, and dribbling after voiding; Gravida 3, Para 3, Menarche at age 14. Last menstrual period (LMP) 1 1/2 years ago; sexually active but experiencing dyspareunia
Mental Status: Case of insomnia, increased fatigue, and feeling somewhat depressed
Advanced Practice Nursing Intervention
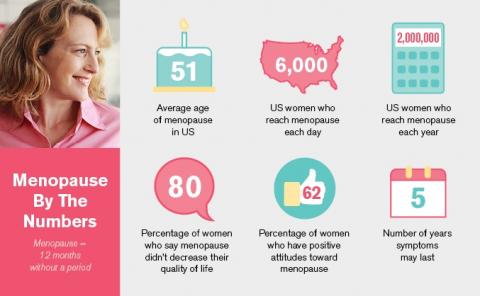
Women experience various symptoms while they reach menopause. For instance, one can experience hot flashes, genital skin, insomnia, loss of sexual zeal and vaginal changes. Menopause occurs naturally due to old age and failure in ovulation. Normal menopause occurs between forty five and fifty years. However, there are cases of premature menopause where it happens before forty years.
Menopause is considered as a natural event and it is clear that every woman will have to go through it someday. However, medical intervention is necessary where the post menopause symptoms go on for few years after the last period. Most of these patients experience hot flushes, sweats and other symptoms such as fatigue, headaches, lack of sleep, loss of sex drive and depression (Finkler, 2012).
Long-term changes after menopause include hair and skin changes. After menopause, most women tend to lose their level of skin collagen. This leads to dry, thin and itchy skin. Further, they experience genital area changes such as vaginal changes, vulva changes and increased frequency of urination. Moreover, females experience signs of osteoporosis after menopause. Osteoporosis is a condition where the bones become less strong and less dense. Thus, this condition may cause the bones to fracture easily. Consequently, post-menstrual risks include the increase in the risk of developing cardiovascular disease (Clouse & Sherif, 2010).
In the clinical situation, the doctor will initially carry out various vital tests to diagnose the cause of the condition. One of the most common tests in this condition is the hormone blood tests. This is used to confirm that the patient is experiencing menopause. Further, the hormonal tests can provide useful information regarding the condition of the patient after menopause.
Menopause is considered as a natural occurrence and most patients go through it without medication. However, the short-term symptoms may become severe in some patients. Thus, hormone replacement therapy is provided to women who experienced increased menopause symptoms (Finkler, 2012).
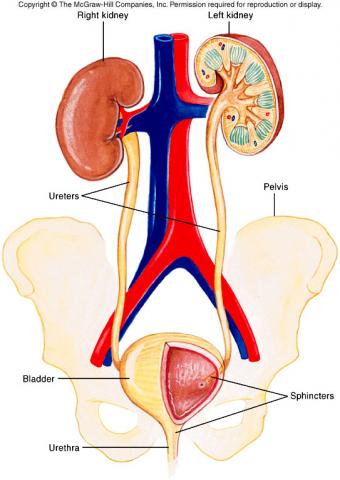
Urine and Blood Levels
Urine and blood tests would be necessary to evaluate the level of LH, FSH and estradiol in menopause. The LH and FSH levels are used to examine menstrual irregularities. If the patient has poor ovarian cycle or past menopause, the level of LH is measured by administration of gonadotropin releasing hormone. Further, a pelvic exam would be necessary to measure the vaginal changes caused by reduction of the estrogen levels. Consequently, bone density tests should be carried to measure the level of osteoporosis.
Hormone replacement therapy
All hormone replacement hormones involve use of oestrogen hormone. Hormone replacement therapy mainly focuses on providing additional oestrogen that ovaries do not provide after menopause. Hormone therapy is available in numerous forms. For example, one can get the therapy in form of tablets, vaginal ring, skin patches, nasal spray and gels. This therapy offers a variety of brands for each of these forms. They all add oestrogen into the patient’s blood stream.
Nevertheless, the use of hormone replacement therapy has some dangers as well. For instance, the use of this therapy increases the risk of patients developing uterus cancer. Thus, oestrogen in this therapy is combined with progestogen hormone. This reduces the risk for one developing uterus cancer (Fogel & Woods, 2013).
Hormone replacement therapy is available in two types of combination therapy. Monthly cyclical hormone replacement therapy and three month cyclical hormone replacement therapy. Monthly cyclical hormone replacement therapy entails taking oestrogen daily and progestogen added after every fourteen days, for a 28 day treatment cycle. On the other hand, three months cycle entails taking oestrogen daily and progestogen after fourteen days for three weeks. However, if the patient has stopped experiencing her periods for a year or more, then she will be advised to take a daily combination of oestrogen and progestogen daily (Clouse & Sherif, 2010).
Vaginal symptoms
Vaginal symptoms caused by low levels of oestrogen include, atropic vaginitis and vaginal dryness. This often occurs in post-menstrual patients and it leads to pain experienced during sex. The condition is managed by hormone-replacement therapy and through application of non-hormonal lubricants and mosturisers.
Lifestyle changes
Postmenstrual patients usually experience osteoporosis, which put them in danger of losing bones or getting fracture easily. Thus, various lifestyle changes are necessary to increase the efficiency of their bones. Physicians advise women undergoing menopause to avoid smoking, get enough calcium, avoid caffeine, avoid alcohol, avoid spicy foods, get vitamin D, maintain healthy weight and exercising frequently. Further, these patients are advised to eat healthy foods that are low in fat and high in fiber.
Further, the patient should be referred to a dietician to improve the patient’s food choices. For instance, the patient needs to stop taking 12 cokes a day. Caffeine and sodas can increase the degree of hot flashes experienced by the patient.
Medical management
The patient should continue using medications prescribed in order to reduce the previously diagnosed conditions from reoccurring. Further, the patient should engage in a hormone replacement therapy where she would take both oetrogen and progestogen daily. This is because she stopped having periods more than a year ago. Further, her lipid profile should be watched closely since she was previously diagnosed with hyperlipidimia (Fogel & Woods, 2013).
Moreover, the medications should include vitamin supplements and antidepressants prescriptions. Antidepressants such as effexor, paxil and Prozac grabapentin help reduce hot flashes.
References
Finkler, K. (2012). Women in pain: Gender and morbidity in Mexico. Philadelphia: University of Pennsylvania Press.
Clouse, A. L., & Sherif, K. (2010). Women's health in clinical practice: A handbook for primary care. Totowa, N.J: Humana Press.
Fogel, C. I., & Woods, N. F. (2013). Women's health care in advanced practice nursing. New York: Springer Pub.
Subjective Data:
Client Complaints:
 The patient complains that he is experiencing a decreased urinary flow. He explains that that he has recently experienced increased nocturia and his strength in urinary flow has decreased. He is currently complaining of increased nocturia condition. He explains that he is currently experiencing high urination frequency where sometimes he uses the bathroom four to five times a night.
The patient complains that he is experiencing a decreased urinary flow. He explains that that he has recently experienced increased nocturia and his strength in urinary flow has decreased. He is currently complaining of increased nocturia condition. He explains that he is currently experiencing high urination frequency where sometimes he uses the bathroom four to five times a night.
HPI (History of Present Illness):
The patient asserts that he has experienced the condition for the last two years. Consequently, he explains that he has never sought for medical help before. However, the previous condition was less severe, and the past two weeks the condition has become complicated. The condition is now severe as he experiences increased nocturia and slight terminal dysuria.
PMH (Past Medical History—include current medications, any known allergies, any history of
Surgery or hospitalizations):
The patient’s past medical history shows that he has been diagnosed with hypertension and hypercholesterolemia in the past. Furthermore, the patient has been hospitalized of a suspected angina case before. However, the condition was diagnosed as chest wall syndrome. He has never has surgery before. The current medication prescription for the patient includes cardizem 240mg daily and zocor 20mg daily. Further, the patient has no known drug allergies.
Significant Family History:
Social/Personal History (occupation, lifestyle—diet, exercise, substance use)
The patient is a professional engineer holding a master’s degree in engineering. He has no financial problems and he has a good access to healthcare services. He has a family but two grown up children and his wife. He lives with his wife who is of sound health. Moreover, the patient has one sister and one brother who are well and alive. There is a remote history of heart disease among his uncles and aunts. His support system comprises of his wife and his friends from work. The patient denies any substance abuse. He does not take cigarettes and he does not drink alcohol. His wife does most of the cooking and the patient believes that he eats healthy. Further, he explains that he gets adequate exercises and maintains a regular check up regime with his physician.
Description of client’s support system:
The client has a strong support system comprising of his wife and friends. His wife is in a healthy condition and she offers wide levels of support to her husband. Further, his friends from work also give support to the patient. However, the patient does not receive support from his local community. He has no relationship with his local community.
Behavioral or nonverbal messages:
The patient seems positive about his condition. He does not seem stressed about his condition. However, he is a little uncomfortable with his frequent urination situation.
Client awareness of his/her abilities, disease process, healthcare needs
The patient is aware of his need to follow prescription. He currently follows his previous medications keenly and he understands why he has to do so. Consequently, the patient is quite positive about his healing process. He believes that with the right medical care, he can recover from the condition. However, the patient portrays poor levels of cognitive measures. For instance, he has a good access of medical care, but he never seeks medical help until the it is an emergency situation.
Objective Data:
Vital signs
Vital Signs: BP right arm sitting 140/92; T: 99 po; P:80 and regular; R 18, non-labored;
SubT
Physical assessment
Wt: 200#; Ht: 71”
HEENT: WNL
Lymph Nodes: None
Lungs: Clear
Heart: RRR with Grade II/VI systolic murmur heard best at the right sternal border
Carotids: No bruits
Abdomen: Android obesity, non-tender
Rectum: Stool light brown, heme positive. Prostate enlarged, boggy and tender to
palpation.
Genital/Pelvic: Circumcised, no penial lesions, masses, or discharge.Testes are
descended bilaterally, no tenderness or masses
Extremities, Including Pulses: 2+ pulse throughout, no edema in the lower legs.
Neurologic: Not examined
Lab Results/Radiological Studies/EKG Interpretation
Lab Results
PSA: 6.0
CBC: WNL
Chem panel: WNL
Radiological Studies: None
EKG: None
Client’s Support System as Perceived by Healthcare Professional
The client has a strong support system. His wife plays central to his support system and his friends from work. However, the patient only relies on his wife and his friends from work for support. Thus, he should establish relationships with his neighbors and the local community for more support.
Client’s locus of control and readiness to learn as perceived by Healthcare Professional
The patient has taken his previous diagnoses carefully and his lotus of control seems positive. However, the patient requires wide levels of patient education regarding healthy practices. The patient widely believes that he is healthy and he never seeks medical help regularly.
Diagnoses/Client Problems (include medical diagnoses):
The client’s problems include the previous medical diagnoses of hypertension, hypercholesterolemia and urinary tract infection and disorder. Further, the patient has a prevailing condition of chest wall syndrome, which is now managed after successful diagnosis.
Advanced Practice Nursing Intervention Plan including Interdisciplinary Collaboration and Community Resources and Plan for Patient Follow up:
The treatment plan for the dysuria patient should incorporate wide aspects of drug treatment, and urinary retention therapy. Consequently, the medical practitioner would consider collaborating with various professionals such as physicians to manage the condition. Further, follow-up measures should be set up after the patient discharge to ensure the effectiveness of the patient and to avoid the condition from occurring again in the future.
Urinary retention therapy
After establishing the cause of the dysuria condition, the medical practitioner should consider engaging the patient in a urinary retention therapy to repair the tissue damage caused by the infection. For instance, renal impairment may be cause renal tissue damage. Thus, after establishing the disease, the medical practitioner should carry out a tissue repair treatment on the patient. Urinary therapy mainly focuses on ensuring the patient resumes the right flow-rate and urinal frequency (Ajithkumar, 2012).
Nocturia is an impairment in the urinary rate of flow. The nocturia condition is caused naturally by age. Older people normally experience nocturia because of the reduction in the strength of their urinary tract function. However, the condition poses a lot of challenges including health problems such as dehydration and it lowers the quality of life. In normal situations, nocturia is easily managed by the patient and they can easily adjust to the increased urge for urination. However, if the condition is unmanageable or it has reached emergency levels, medical help is necessary.
The medical condition experienced by the patient is global polyuria. Polyuria is the excessive production of urine, which is not limited to sleeping hours. The major causes of polyuria is diabetes and primary thirst disorders. Further, the condition can be caused by the deficiency of the antidiuretic hormone and the malfunction of the hypothalamus neurons (Weiss, 2012).
In order to maintain the nocturia condition of the patient, it is necessary to evaluate the risk causing factors. The rick causing factors to the condition include diabetes, age, urinary tract disorder and excessive intake of fluids. According to the patient’s condition, age might be one of the reasons leading to the condition. However, the condition seems more complicated. There might be chances of urinary tract disorder for the patient’s condition. Thus, a problem-based diagnosis important to establish the cause of the urinary tract disorder (Buttarp, Trybulski, Polgar & Sandberg-cook, 2013).
The medical practitioner in this clinical situation should asses the previous medical history of the condition, asses any voiding behavior and asses any chances of neurological disorder. In order to evaluate whether there are any chances of urinary tract infection, it is necessary to carry out a urine test on the patient. Further, the patient should undergo screening for edema, and the medical practitioner should also evaluate the age-related factors of the condition. Nevertheless, the condition may result from prolapse. Consequently, a neurogenic examination is vital to assess the tone of the anal sphincter (Weiss, 2012).
Management of the condition
Management of the condition can be achieved by using various approaches. Lifestyle changes are necessary in managing the condition. Changes in lifestyle factors such as alcohol and caffeine intake are important in reducing the prevalence of the condition. Further, fluid restriction is important to reduce the intensity of the nocturia condition.
If the condition is severe the medical practitioner can carry out a surgical operation on the patient to evaluate the level of damage and manage the level of tissue damage. Drug prescription should include antidiuretic drugs such as desmopressin. Desmopressin is the most prescribed antidiuretic drug in cases of nocturia. Nevertheless, if the condition is caused by the overreaction of the bladder, antimuscarinic drugs are appropriate. Antimuscarinic drugs incluse solifenacin, darifenacin and oxybutynin help improve the bladder condition (Weiss, 2012).
Further, patient education is necessary to establish cognitive measures for the patient. For instance, the patient should be advices on the right level of fluid intake and the right urination patterns to avoid sleep interference. Further, sleep and rest therapy are important for the patient. This is because the nocturia condition may affect the rest period, which may lead to a poor work performance and body fatigue.
References
Ajithkumar, T. V. (2011). Oxford desk reference. Oxford: Oxford University Press.
Buttarp, M., Trybulski,J., Polgar, B, P., Sandberg-cook, J., (2013). Primary Care. Elsevier Health Science Division ISBN: 9780323075015.
Weiss, J. P. (2012). Nocturia: Causes, consequences and clinical approaches. New York, NY: Springer.
Patient initials: D.C
Age: 68y/o
Gender: male
Subjective data:
Client complains
 The patient complains that he feels weak, feverish and he has short breath. Further, he explains that he has been coughing up yellowish sputum. He complains that the cough has increased over the past few days, and he experiences chest pains when coughing. He describes the chest pains as “stabbing knife” like pain on his right side.
The patient complains that he feels weak, feverish and he has short breath. Further, he explains that he has been coughing up yellowish sputum. He complains that the cough has increased over the past few days, and he experiences chest pains when coughing. He describes the chest pains as “stabbing knife” like pain on his right side.
History of present illness
The patient has had cold for the last two weeks. The cold has progressed over the two weeks from his head to his chest.
Past medical history
The patient has been previously diagnosed with hypertension x fifteen years ago. Moreover, he has had a right knee surgery after injury obtained while skiing eight years ago. However, he has healed and no residual problems.
Social history
The patient is a retired university professor. He is married to three adult children and two grandchildren, who are well and healthy.
Family history
The patient’s mother died of lymphoma at the age of eight years. His father, aged ninety-two, has been previously diagnosed with cardiovascular accident (CVA) three years ago. Further, the patient’s father suffers from hypertension.
Physical assessment findings
General: Pleasant man, appearing stated age; breathing is labored and patient appears to be in moderate distress
Vital signs
Temp: 102.5 oF; HR: 80 bpm; BP: 125/78 mmHg; RR: 32 bpm; Wt: 195 lbs; Ht: 6'1"
CNS: Alert & Oriented X 3
Head, eyes, ears, nose, and throat (HEENT): PERLA, tympanic membranes intact, mucus membranes red and wet; throat erythematous, no exudates; mild bruits noted on the neck
Pulmonary: Slight splinting on left side with inhalation; crackles and rales in left lower base; O2 saturation: 88 percent
Cardiovascular: PPP, NSR, S1, S2, no S3 or S4
Lab findings
WBC: 18 X 103 cells/mm3
Neut: 85 percent
Bands: 6 percent
Lymph: 8 percent
HgB: 12 mg/dL
HCT: 40 percent
Na+: 140mEq/L
K+: 4.5 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
BUN: 11 mg/dL
SCr: 0.6 mg/dL
Blood glucose: 138 mg/dL
ABG: pending
Cultures: Blood culture: pending sputum culture; gram stain: < 10 epithelial cells, culture pending
Radiology: CXR: Left lower lobe (LLL) consolidation
Medications (prior to diagnosis)
Hydrochlorothiazide 25 mg po daily
Metoprolol 50 mg po bid
Sertraline 50 mg po daily
ASA 325 mg po daily
Acetaminophen 500 mg po 2 tabs 1-2 X per week for headaches, aches, and pains
Allergies: Amoxicillin—nausea and diarrhea
Immunizations: None in the past ten years
Diagnoses/client problems
Community acquired pneumonia
Hypertension currently controlled
Measures BP once every two weeks with home BP monitor—always between 120–140/70–80 mmHg; no need to work up on palliative care for advanced disease (PCAD)
Medications after diagnosis
Oxygen 2L via nasal prongs
Acetaminophen 325 mg 2 tabs po q4H p.r.n; temp: 98 oF (Max 4000 mg per twenty-four hours)
Hydrochlorothiazide 25 mg po daily
Metoprolol 50 mg po bid
Sertraline 50 mg po daily
ASA 325 mg po daily
Substance abuse
The patient is a non-smoker. However, he admits to taking 1-2 glasses of red daily.
Advanced practice nursing intervention plan
Pneumonia is a serious respiratory disease that causes an inflammatory in the lung tissues. The disease is usually caused by virus or bacteria, which are normally present in the environment. The disease occurs when one inhales air with virus, bacteria or other germs. Normally, pathogens that enter the body through the respiratory tract are trapped in the sputum, and killed by the immune system. However, when individuals grow old, the strength of their immune system reduces substantially. Thus, pneumonia causing pathogens appear more prevalent among older people. Nonetheless, pneumonia also affects healthy people if they are exposed to these pathogens (Buttarp, Trybulski, Polgar & Sandberg-cook, 2013).
Pneumonia signs and symptoms include shivers, cough, sweats, fever, lack of appetite and feeling weak. In some cases, pneumonia patients exhume yellow colored sputum, which sometimes may become bloodstained. In addition, patients suffering from pneumonia may become breathless or breathe fast. The chest may get tight and in some situations, sharp chest pains may occur (Buttarp, Trybulski, Polgar & Sandberg-cook, 2013).
If the disease is not fully developed, it can be treated at home. Antibiotics such as amoxicillin can reduce the prevalence of the disease. Further, in a home environment, pneumonia patients can engage in various practices that will help reduce the prevalence of the disease. For example, patients suffering from the disease should drink lots of water and take paracetamols to reduce headaches and fever. Moreover, if the disease is mild, over the counter drugs can be beneficial to the patient.
In clinical treatment, chest x-rays are used to show the prevalence of the disease. Consequently, sputum and blood tests are used in the laboratory to determine which pathogen is causing the disease. After establishing the pathogen, medical practitioners will decide which antibiotic will be used. In serious cases, supportive treatments such as oxygen supply are necessary if it is an emergency pneumonia case (Rush, 2007).
Community acquired pneumonia is mostly caused by pathogens including streptococcus pneumonia, moraxella catarrhalis and haemophilus influenza. These are the most common pathogens causing community acquired pneumonia (Suttorp, Welte, & Marre, 2011). The risk factors leading to community-acquired pneumonia include; mostly streptococcus pneumonia, influenza and increased prevalence of chronic bronchitis. Laboratory tests for the infection include; chest radiography, sputum culture and blood cultures. Furthermore, other tests such as serum transaminase levels, urinalysis, C-reactive protein levels and cold agglutinin titers are vital in assessing the condition (Fein, 2010).
In order to kill the pathogens causing the condition, antimicrobial therapy is necessary. Antimicrobial therapy entails treatment of infectious diseases by using chemotherapeutic agents. These chemotherapeutic agents kill microbes and interfere with microbial growth. Antimicrobic drugs enable facilitates various procedures in the body, which inhibit further microbial growth. For instance, these drugs help eliminate the pathogen from the host or inactivating the pathogen (Suttorp, Welte & Marre, 2011).
The Clinical Situation
In a clinical situation, D.C patient situation, one of the most available microbial therapies is empiric therapy. First, the clinical practitioner asses the physical conditions of the patient. This may require admission of the patient to an acute care hospital. During this admission, primary health aspects are evaluated on the patient.
If community acquired pneumonia is detected or suspected, then the medical practitioner analyzes what type of pathogen has caused the condition in order to administer the right drug therapy. There are two types of pathogens that cause community acquired pneumonia; atypical and typical pathogens.
After the detection of the pathogen, medical therapy is necessary to reduce the growth of the pathogen or worsening of the condition. if the patient has no comorbities, then the following drugs will be advised. Azithromycin ½ mg PO One dose the first day, then 1/4mg PO daily for four days. Further, clarithromycin ½ mg PO or alternatively an extended release on 1000mg PO for twenty-four hours will be advised. In addition, Doxycycline 100mg will be advisable on a PO bid.
If these antibiotics fail to react positively within three months, then further drug therapy is necessary. Amoxicillin or amoxillin-clavulanate 2g Po for 12 hours is advisable added on the azithromycin or clarithromycin prescription.
If comorbites are present on the patient, the levoflaxacin and moxifloxacin prescription are advisable. Levofloxacin prescription should be 750mg PO for 24hours or IV. Consequently, the moxifloxacin prescription should be 400mg PO for twenty-four hours or IV. A combination of of beta-lactams can be used in case of a drug resisting pathogen. This drug therapy should take not less than five days. During the therapy, the patient’s conditions should comprise of a stable blood pressure and air oxygen in the room greater than 90percent saturated.
However, antimicrobic drugs function according to the range of spectrum activity. Some of these drugs target lesser pathogens and they may fail to eliminate the pathogen causing the disease. Further, these drugs have various side effects. For example, they may increase the toxicity to the host or allergic reactions. Nevertheless, if the antimicrobial therapy is accurate, the action of the drugs will be less toxic to the host because of selective toxicity (Campbell, 2009).
References
Fein, A. (2010). Diagnosis and management of pneumonia and other respiratory infections. Caddo, OK: Professional Communications.
Campbell, G. D. (2009). Contemporary diagnosis and management of community-acquired pneumonia. Newtown, Pa: Handbooks in Health Care Co.
Suttorp, N., Welte, T., & Marre, R. (2011). Community-acquired pneumonia. Basel: Birkhäuser Verlag.
Buttarp, M., Trybulski,J., Polgar, B, P., Sandberg-cook, J., (2013). Primary Care. Elsevier Health Science Division ISBN: 9780323075015.
Rush, B. (2007). Equine Respiratory Diseases. Oxford: John Wiley & Sons.
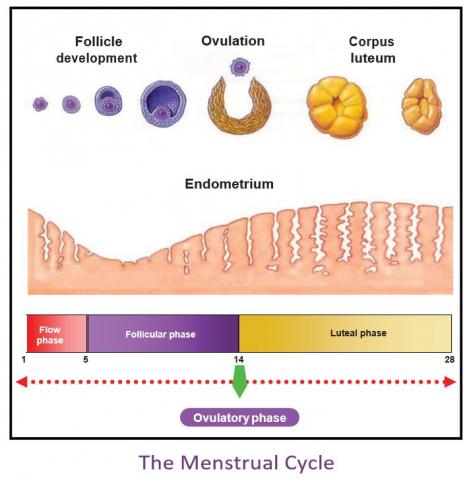 The menstrual cycle occurs regularly after a period of 28 days. There are various hormonal responses produced in a normal menstrual cycle. The anterior lobe in the pituitary gland induces hormonal responses in the ovaries, during menstruation. Hormones secreted during ovulation are the gonadotropic hormones. The gonadotropic hormones consist of luteotropic hormone, luteinizing hormone and the follicle-simulating hormone.
The menstrual cycle occurs regularly after a period of 28 days. There are various hormonal responses produced in a normal menstrual cycle. The anterior lobe in the pituitary gland induces hormonal responses in the ovaries, during menstruation. Hormones secreted during ovulation are the gonadotropic hormones. The gonadotropic hormones consist of luteotropic hormone, luteinizing hormone and the follicle-simulating hormone.
The follicle-simulating hormone (FSH) is highly secreted during the first half in the menstrual cycle. The follicle- simulating hormone induces the ripening of the ovulation and follicle. The luteinizing hormone is produced at the mid of the menstrual cycle. Similarly, it also induces the ripening of the ovulation and follicle. The luteotropic hormone (LTH) maintains the corpus luteum. The secretion of the luteotropic hormone during ovulation does not occur in all animals. The follicle-simulating hormone and the luteinizing hormone are the main hormones during ovulation. In some cases, the two main hormones are induced to women experiencing infertile ovulation (Porth & Matfin, 2009).
The secretion of the menstrual hormones is controlled by the pituitary glands. The pituitary glands produce estrogen and progesterone to control the production of the luteinizing hormone and the follicle-simulating hormone. Estrogen inhibits the output of the follicle-simulating hormone form the pituitary glands. On the other hand, the secretion of the luteinizing hormone is controlled by progesterone. Thus, the pituitary glands stimulate the ovary during ovulation, and then the ovary inhibits the pituitary. The hypothalamus controls the general functions of the pituitary glands (Porth & Matfin, 2009).
What are the risk factors in the development of breast cancer?
The risks experienced in the development of breast cancer involve both preventive and unpreventable factors. The preventive factors involve weight, exercise, unhealthy food and smoking cigarettes. Breast cancer is more prevalent in overweight persons. Further, lack of exercises may affect one with the risk of suffering breast cancer. Consumption of unhealthy foods and cigarettes accelerates the chances of one getting breast cancer.
Unpreventable factors causing breast cancer include gender, family history, genetics and age. Breast cancer is more prevalent on the female gender than on the male gender. An individual’s genetic family history can affect the chances of the individual suffering from breast cancer. For instance, if one of your close relatives has previously been diagnosed with breast cancer, then there is a high risk of you suffering from breast cancer in the future. In addition, an individual’s genetic structure may affect the prevalence of breast cancer upon the individual. Abnormal hereditary genes from parents to children may induce breast cancer (Anders & Lin, 2012).
How have the results of the Women’s Health Initiative changed treatment of menopause in women?
The Women’s Health Initiative has changed the treatment of menopause in women in various ways. The most functional treatment initiated by the Women’s Health Initiative is the menopausal hormone therapy. The menopausal hormone therapy treatment is for women undergoing menopause to reduce the adverse symptoms of menopause. Menopause causes various biological changes such as bone loss caused by low levels of the hormones estrogen and progesterone (Carlson, Eisenstat & Ziporyn, 2004).
The hormones used in the menopausal hormone therapy are different from normal body hormones because they are produced from various animals and plants. In addition, some of these hormones are produced in the laboratory. However, the structure of the hormones is similar but not identical to normal body hormones.
References
Porth, C.M., & Matfin, G. (2009). Pathophysiology: Concepts of altered health states. (Eight ed.) Philadelphia, PA.
Carlson, K. J., Eisenstat, S. A., & Ziporyn, T. D. (2004). The new Harvard guide to women's health. Cambridge, Mass: Harvard University Press.
Anders, C. K., & Lin, N. U. (2012). 100 questions & answers about triple negative breast cancer. Burlington, MA: Jones & Bartlett Learning.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
