+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help in your homework? We offer quality research writing help, All our papers are original, 0% plagiarized & uniquely written by our dedicated Masters specialists. My Essay Services is an experienced service with over 9 years experience in research writing and over 83,000 essays over the years. You will receive a plagiarism check certificate that confirms originality for any essay you order with My Essay Services
Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help in your homework? We offer quality research writing help, All our papers are original, 0% plagiarized & uniquely written by our dedicated Masters specialists. My Essay Services is an experienced service with over 9 years experience in research writing and over 83,000 essays over the years. You will receive a plagiarism check certificate that confirms originality for any essay you order with My Essay Services
 Poly-pharmacy refers to the use of multiple medications or the use of medicine that is not indicated for a disease condition or the ineffective or inappropriate use of medications than they are medically necessary (Hilmer et al. 2009). The use of medicines that constitute therapeutic duplication also amounts to Poly-Pharmacy (Robert et al. 2014). A rise in life expectancy in many regions around the world has resulted in the number of people aged 65 years and above.
Poly-pharmacy refers to the use of multiple medications or the use of medicine that is not indicated for a disease condition or the ineffective or inappropriate use of medications than they are medically necessary (Hilmer et al. 2009). The use of medicines that constitute therapeutic duplication also amounts to Poly-Pharmacy (Robert et al. 2014). A rise in life expectancy in many regions around the world has resulted in the number of people aged 65 years and above.
Older people are more likely to suffer from multiple disease conditions like hypertension, diabetes, cardiovascular diseases, arthritis, and cancer. These conditions require multiple drug therapies for their management and treatment (Hilmer et al., 2004) Poly-pharmacy is, therefore, very more prevalent in older adults. Self-medication and self-prescriptions of drugs and a prescribing cascade also cause poly-pharmacy. A prescribing cascade entails patients take medications and then exhibit the side effects, which are then misinterpreted by the health care professional as a disease symptom. Ineffective communication and coordination between the patients and the health care provider resulting in multiple prescriptions in different healthcare settings is also a major cause of Poly-Pharmacy (Lisa 2008).
In ambulatory care, poly-pharmacy happens when the prescribed medicines are five or more than five types of medicines (Robert et al. 2014). However, current medical practices guidelines usually require multiple medications to treat every condition for optimal clinical benefits and, therefore an elderly patient with two or more disease conditions usually exceeds the ambulatory threshold of fewer than five medications (Richard, 2007).
The degree of poly-pharmacy is influenced by the factors such as age, the natural progression of the disease, hospitalizations or care settings for the elderly (Richard, 2007). According to a survey carried out by Qato et al. in 2006, 37 percent of men and thirty-six percent of women aged 57-85 years of age in the survey used more than five types of medications. The most common type of medications involved in cases of poly-pharmacy are prescription medicines, over the counter medications and dietary supplements (Hilmer et al. 2009). Nearly fifty percent of all old people take one or more type of unnecessary medications (Lisa, 2008).
Whereas poly-pharmacy can be therapeutic and effective in the treatment of multiple illnesses in the elderly, Research has, Clearly established a very robust relationship between poly-pharmacy and some negative clinical consequences (Ann et al. 2003). This review details the adverse health outcomes of poly-pharmacy in old people and highlights the interventions for improving medication use by old people.
The Negative consequences of Poly-pharmacy on older people
1) Adherence
Old patients are at high risk of receiving inappropriate medication and increased cases of adverse drug reactions that influence a patient’s adherence to their medication regimes. Adverse drug reactions result in patients avoiding following the drug intake regimes (Hilmer et al., 2009). Poly-pharmacy results in complex medication regimes that make non-adherence a very common problem among old people with a prevalence rate of fifty percent for the elderly population (Robert et al. 2014).
2) Adverse drug reactions and inappropriate prescribing
Multiple drug prescriptions increase the risk of inappropriate prescriptions that result in adverse drug reactions. Adverse drug reactions increase with an increase in the number of medications taken (Richard, 2007). Adverse drug reactions occur in five to thirty percent of outpatient hospital visits and account for twelve percent of all hospital admissions (Robert et al. 2014).
The risk for development of adverse drug reactions is strongly linked with multiple comorbidities and poly-pharmacy. Lisa (2008) explains that as the body ages, it processes medicines differently. Medicines also stay in the body for longer periods and medicines are highly concentrated in some specific parts of the body due to diminished circulation and reduced cardiac output. Reduced renal and liver functions also influence how drugs are metabolized making old people at a very high risk of suffering from adverse drug reactions (Lisa 2008).
Ann et al.(2003) also explain that delayed stomach emptying and the reduced ratio of body fat to water may also result in altered bio-physiology that make old people unable to tolerate the prescribed medications and experience side effects and adverse drug reactions. Hilmer et al. (2009) assert that the most common drugs associated with adverse drug events in the elderly are anti-coagulants, NSAIDS, Diuretics, Cardiovascular Medications, Antibiotics, Diabetic Medications, Anticonvulsants, and Benzodiazepines.
3) Drug interactions
Old people are more predisposed to drug interactions (Dementra, 2012). The probability of drug interactions increases with an increase in the number of medications with a fifty percent risk when a patient is taking five to ten medications and a 100 percent risk when a patient is taking more than twenty medicines. Many patients are living longer with chronic disease conditions requiring multiple drug therapy, and the risk of drug interactions is a major concern for healthcare professionals (Robert et al., 2014).
4) Geriatric syndromes
Multiple medications are linked to many geriatric issues like urinary incontinence and increased risk of suffering from lower urinary tract infections. Other geriatric syndromes are cognitive impairment and loss of balance that results in fractures and falls (Hilmer et al. 2009).
5) Effects on Morbidity and functional status
Poly-Pharmacy can help in controlling the multiple comorbidities in old people, but it is associated with a decline in the functional status of individuals. Poly-pharmacy usually results in a reduction in the abilities to perform the instrumental abilities of daily living (IADL) and a decrease in the physical functioning of individuals (Robert et al., 2014).
6) Falls
Falls are associated with the reduced morbidity in older people and may be enhanced by taking of certain medications especially the psychotropic and Central nervous system medications. People taking more than two psychotropic agents have a 2 to four-fold risk of falling compared to those taking just one psychotropic agent (Hilmer et al. 2009). As an independent variable, poly-pharmacy appears to be linked to an increase in the risk of falls in old people, but the type of medications taken determines the link between poly-pharmacy and falls. Poly-pharmacy is also a risk factor that exacerbates falls and it is synergized by the other factors associated with poly-pharmacy such as drug-drug interactions and the drug-disease interactions (Ann et al. 2003). Studies have indicated that taking four or more than four types of drugs is associated with increased risk of mild, injurious, and recurrent falls (Zia et al. 2015).
7) Increased healthcare costs
Poly-pharmacy results in an increase in healthcare costs for the patient and the healthcare system (Hilmer et al. 2009: Robert et al., 2014). Some data suggest that poly-pharmacy results in an increase in healthcare costs by thirty percent, due to potentially inappropriate medication prescribing, increased hospital visits and the associated adverse drug reactions associated with poly-pharmacy (Richard, 2014)
9) Effects on Nutrition and feeding patterns
Poly-pharmacy also affects a patient’s nutritional status. Patients taking more than ten medications have poor nutrition and a risk of malnutrition (Robert et al., 2014). Adverse drug effects may also affect the appetite of patients resulting in poor eating habits such as taking unhealthy and unbalanced diet (Ann et al., 2003).
10 Effects on Mortality
Poly-pharmacy is also associated with increased risk of mortality in old patients (Emily, 2007). The adverse medication outcomes associated with multiple drug prescriptions in hospitals is the fourth leading cause of mortality in hospitals (Dementra, 2012).
10) Cognitive impairment
Poly-pharmacy is also associated with an increase in the risk of development of mild cognitive impairments, which is a syndrome characterized by a cognitive decline, which is greater than the age of an individual, education, and a reduction in the ability to do the activities of daily life (Gonzalez, 2014). Cognitive impairments such as deliriums and dementia are also associated with poly-pharmacy. The risk of suffering from deliriums increases with an increase in the number of medications taken (Hilmer et al., 2009). Mild reduction in the cognitive function occurs due to a combination of factors. These factors are reduced, physical activity, comorbidities and declining executive functions associated with age and the use of different and in-appropriate drugs in elderly patients. Poly-pharmacy can exacerbate the decline in the cognitive function of the elderly in the different cognitive domains and the functional independence of a person (Gonzalez 2014).
Poly-pharmacy has some severe negative effects on the health of old people. Health care professionals should lead the fight of this silent epidemic. The strategy that health care professionals can use to reduce cases of poly-pharmacy in old people is a better review of medicines at the time of prescriptions to ensure only the required medicines are administered. Better communication and coordination with old people in the management of multiple illnesses, and educating and supporting patients in self-medication can also help in reducing cases of Poly-pharmacy (Ann et al. 2003).
References
Ann, B. Liz, D. Gillian, L. (2003). ‘Poly-pharmacy and older people.’ Nursing Times, Volume 99, no, 17 (2).1-4.
Dementra, EA. (2012). Poly-pharmacy: A modern day silent epidemic- Signs and symptoms.
Emily, RH. Angela, CC. Joseph, TH. ‘Poly-pharmacy in elderly patients.’
The American Journal of Geriatric Pharmacotherapy, Volume 5, Number 4, 345-352
Gonzalez XA. (2014). "Cognitive decline and poly-pharmacy in an elderly population." Dissertations Paper 517. Retrieved from
Hilmer, SN, Gnjidic D. (2009). ‘The effects of poly-pharmacy in older adults.’ Discovery, Volume 85(1), 84-86.
Lisa, P (2008). ‘Poly-pharmacy and aging: is there cause for concern.’ Gerontology Update 6,
Richard, F., (2007). Poly-pharmacy and the elderly.’ Geriatric Medicine Journal, 41-47.
Robert, LM. Joseph TH, Emily RH (2014). ‘Clinical consequences of poly-pharmacy in Elderly.’ Expert Opin Drug Saf. ; 13(1): 10.1517-1534
Qato DM, Alexander GC, Conti R. (2008). ‘Use of prescription and over-the-counter
Medications and dietary supplements among older adults in the United States.’ AMA; 300:2867–2878.
Zia, A. Kamaruzzaman, SB. Tan MP. (2015). ' Poly-pharmacy and falls in older people: Balancing evidence-based medicine against falls risk.’ Postgrad Med.127 (3) 330-337.
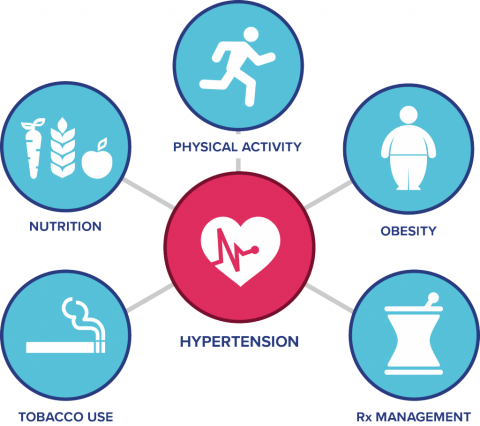 Hypertension (also called blood pressure), is a multifactorial disorder that involves some abnormalities in the functioning of the heart and its components and as well kidneys (Benhagen, 2005). There are different types of hypertension depending on the cause and the significant impact that it has on the victim. Primary hypertension (also called essential hypertension) is the most common hypertension affecting different people. It does not have a known cause. The other type is secondary hypertension. With the later type, it appears because of reversible factors, and in most cases it is curable. Other types include; malignant, isolated systolic and resistant hypertension. The paper focuses on hypertension discussing the risk factors attributed to the condition (Buttaro, 2013).
Hypertension (also called blood pressure), is a multifactorial disorder that involves some abnormalities in the functioning of the heart and its components and as well kidneys (Benhagen, 2005). There are different types of hypertension depending on the cause and the significant impact that it has on the victim. Primary hypertension (also called essential hypertension) is the most common hypertension affecting different people. It does not have a known cause. The other type is secondary hypertension. With the later type, it appears because of reversible factors, and in most cases it is curable. Other types include; malignant, isolated systolic and resistant hypertension. The paper focuses on hypertension discussing the risk factors attributed to the condition (Buttaro, 2013).
1. Risk factors that can lead to blood pressure elevation
As stated earlier, hypertension is among the most complex disorders experienced by many people. There are many risk factors attributed to the prevalence of the disorders among many people. Some of the risk factors include:
A). Salt sensitivity- among many hypertension victims, their bodies have a negative response to sodium intake. Increase in sodium capacities in the body than the kidneys can excrete causes vascular volume to expand (Nadar, 2009). As a result, there is secondary movement of fluids into the intra-vascular region. On the other hand, arterial pressure and heart output increases. Therefore, there is an increase in blood pressure following the increase in heart output (Buttaro, 2013).
B). Age- in many cases, hypertension affects aged people. As a risk factor of hypertension, it has an attribute to the reduction of vascular performance. This is due to the stiffening of arteries. More so, this leads to increase in the blood pressure as the pulse rate increases due to the stiffness of the arteries. Patients suffering from hypertension resulting from age also suffer from the reduction of glomerular filtration rate (Schachter, 2004).
C). Obesity- this has an effect of increasing the risk of elevating blood pressure. According to medical reports, two-thirds of patients suffering from hypertension have a characteristic of having excess weight (Nadar, 2009). This is among teens and as well among aged victims. Hypertension is common in people having a body mass index that is above 25. Two mechanisms explain the link between hypertension and blood pressure. These include; activation of the sympathetic nervous system responsible for originating the heartbeats and as well activation of the renin-angiotensin-aldosterone system (Benhagen, 2005).
D). Smoking- this is another risk factor of elevation of blood pressure. Smoking has an effect of causing cardiovascular disorders. This on the other hand has a significant effect on the blood pressure of the victim as the performance of the cardiac system gets interrupted due to the disorders (Schachter, 2004).
E). Genes- this is another prevalent risk factor of hypertension. Gene such as angiotensinogen (AGT) has a direct link with hypertension. Increase in AGT levels in the human body has an effect of increasing blood pressure and therefore leading to hypertension.
2. How interdisciplinary collaboration can reverse these modifiable risk factors enhancing the healthcare of patients and benefit healthcare providers.
Obesity, attributed as one risk factor to hypertension, remains as a major concern among many people following the effect it has on the human body. BMI-CAD Collaboration Investigators conducted an analysis of research with over 300,000 participants. Participants in the research were obese and were at great risk of suffering from blood pressure related disorders compared to participants with normal body mass index. Results revealed that obese people at higher risk of suffering from hypertension. As a result, they concluded that patients suffering from hypertension should engage in activities that enable them to lose 5-10% of their weight as it can lower their blood pressure (Buttaro, 2013).
Nutrition therapy is another collaborative strategy used in controlling hypertension. The Nutrition Committee of the American Heart Association has dietary guidelines aimed at promoting healthy dietary habits for patients suffering with heart-related disorders including hypertension. As with the strategy, it focuses on achieving and maintaining a healthy weight through the intake of appropriate choice of foods. This is a collaborative measure useful for hypertension patients as it gives them a guideline of dealing maintaining a healthy body size and intake of appropriate choice of foods (Schachter, 2004).
Diagnostic and laboratory assessment are clinical collaborations that are significant in dealing with the cases of hypertension in victims (Nadar, 2009). Through this collaborative measure, it aims at investigating the main cause of hypertension. This on the other hand brings about to a clinical measure of dealing with hypertension. This is an important collaboration as it gives healthcare providers information on drugs to administer to their patients and as well mechanism of dealing with its prevalence (Benhagen, 2005).
Lastly as a collaborative measure for patients with hypertension, they should have an opportunity of expressing their feelings about the disease and as well its treatment to others in the society. This collaborative healthcare measure can assist healthcare providers in their activities and as well while dealing with the disorder (Buttaro, 2013).
3. Education plan for patients reverse these modifiable risk factors
For patients suffering from hypertension, there is a need for the action plan to reduce the prevalence of their condition (Nadar, 2009). The following strategies can play a role as an education plan of reversing the modifiable risk factors;
1. Routine measure of body mass index at each regular body check-up
2. Patients should increase their physical activities
3. Reduction of calorie-rich foods would prevent cases of obesity and as well play a role in reducing the body mass index.
4. Patients should stop and avoid smoking as it is a risk factor of hypertension. This is through encouraging the patient to quit smoking. Attaining this is by highlighting to them the risks that result from smoking tobacco.
5. Lastly, the patient should avoid intake of high quantities of salt.
References
Benhagen, E. F. (2005). Hypertension. New York: Nova Science Publishers.
Buttaro, T. M. (2013). Primary care: A collaborative practice. St. Louis, Mo: Elsevier/Mosby.
Schachter, M., & Monkman, D. (2004). Hypertension. Edinburgh: Elevier Churchill Livingstone.
Nadar, S., & Lip, G. Y. H. (2009). Hypertension. Oxford: Oxford Univ Press.
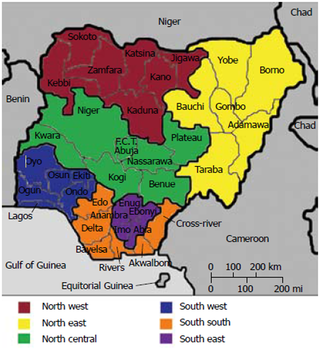
Initial phase
A formative research was conducted to identify factors that pervade screening and therapy for hypertension. This guided our research in the community base risk assessment. Community contributors came from spiritual leaders, hairdressers and survey from community members. The subjects participating in this research were profiled to include male and female Nigerian immigrants, residents of East New York part of Brooklyn and between 25 to 40 years of age. Participants were expected to answer the following survey questions; using a self-reported survey on blood pressure readings, do you have HTN? what do you think are the effects of HTN on daily life? What is your perceived treatment? Participants were given free pens and t-shirts to act as incentives for them to spare some time and participate. The appropriate place to reach this target population was at churches, mosques, Nigerian- restaurants and Nigerian-owned beauty shops.
Intervention
Some important interventions include; key stakeholders must be incorporated into the study such as the office of minority health. Research indicates that there’s low awareness of the risk and serious nature of HTN. Churches and mosques-based community workshops to engage the community on HTN risk, treatment options and monitoring as Nigerians are more likely to associate with a religious group. Outreach volunteers must be nurses from the Nigeria immigrant community as they can likely gain the trust of the community. Funding can be raised through stakeholders.
References
Grey S. Health Risks, Nutrition Assessments and Disease Prevalence among African Immigrant Groups in Atlanta Georgia.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
