+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help write your essay or research? We offer premium quality essay writing help. All our papers are original, 0% plagiarized & uniquely written by our dedicated Masters specialists. My Essay Services is an experienced service with over 9 years experience in research writing of over 97,000 essays over the years. You will receive a plagiarism check certificate that confirms originality for any essay you order with My Essay Services. Fill the calculator on your right to begin placing your order now!
Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help write your essay or research? We offer premium quality essay writing help. All our papers are original, 0% plagiarized & uniquely written by our dedicated Masters specialists. My Essay Services is an experienced service with over 9 years experience in research writing of over 97,000 essays over the years. You will receive a plagiarism check certificate that confirms originality for any essay you order with My Essay Services. Fill the calculator on your right to begin placing your order now!
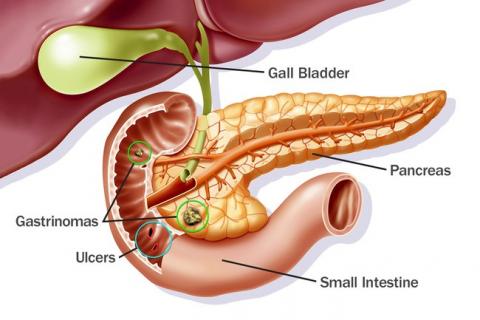 Pressure ulcer is an injury localized on the skin or in the skin’s underlying tissues. The ulcer is caused by pressure resulting from a bony prominence or friction. Most parts of the human body are prone to pressure ulcers. Further, patients diagnosed with impaired mobility are highly susceptible to developing pressure ulcers. In addition, other predisposing factors to development of the condition include poor sensation, fecal incontinence and poor nutrition.
Pressure ulcer is an injury localized on the skin or in the skin’s underlying tissues. The ulcer is caused by pressure resulting from a bony prominence or friction. Most parts of the human body are prone to pressure ulcers. Further, patients diagnosed with impaired mobility are highly susceptible to developing pressure ulcers. In addition, other predisposing factors to development of the condition include poor sensation, fecal incontinence and poor nutrition.
This essay aims at developing a continuous improvement initiative for the pressure ulcer treatment measures. The pressure ulcers are characterized by a three phase healing process. The wounds formed in pressure ulcers patients develop after the inflammatory phase, proliferative phase and matrix formation phases are completed.
Boundaries of the Process
The process to be improved is the treatment of pressure ulcers. The treatment process begins in the inflammatory phase where the skin injury is formed. Consequently, the treatment process ends with the matrix formation. Therefore, treatment options are tailored to suite the patients’ medical needs. For instance, if the disease was identified in its early stages, the treatment process is less complicated.
The currently available patient care plan for pressure ulcers entails treatment of the underlying causes, debridement to remove the contaminated tissues and necrotic tissues, dressing to provide the wound with the optimal healing conditions and frequently turning the pressure ulcers patients to gain pressure relief. Moreover, application of topical biologic agents and nutritional support are also helpful in the patient healing process. The pressure ulcer management plan begins with the cleansing of the wounds, debridement, dressing of the wounds, biological therapies, pressure relieving the affected areas, physical therapies, nutritional therapies and involvement of a multidisciplinary wound care experts.
The Primary Customer
The primary customer in the pressure ulcers is the patients. This is because all efforts are designed to enable the patient recover. The secondary customers are the family members who are also regarded in the patient decision-making plan. For instance, family members may include close relatives, friends and parents in cases of young patients. Patients present to clinical settings with diverse medical needs. For pressure ulcers patients, the patients evaluate the key quality characteristics of the healthcare before engaging in a patient management plan.
Key Quality Characteristics
The key quality characteristics valued by patients include time. Time is very crucial as a measure of service delivery and satisfaction. Most pressure ulcer patients require adequate care provided efficiently. Therefore, most patients will avoid clinical settings that are overpopulated with inadequate staff. This is because pressure ulcers patients require a variety of recovery management plans specifically tailored for their individual health needs. Further, patients require professional services to achieve quality treatment with no health complications. Thus, patients are interested in knowing the professional status of the healthcare providers before engaging in a management plan.
Reducing Medical Errors (Research Indicator)
The pressure ulcer patients encounter physical difficulties and pains. These patients encounter wide levels of discomfort. Thus, another major key quality characteristic assessed by patients before engaging in a treatment plan is the value of care plan provided. Patients require a well detailed, presented and properly monitored care plan to achieve quick recovery. Moreover, there should be an interdisciplinary responsibility provided to pressure ulcer patients because of the complexity of their condition. This requires collaborative patient care services by dietary staff, occupational and physical therapists among other health care services.
The level of information technology efficiency employed by healthcare providers is essential in determining patient demand for their services. For example, some facilities offer innovative electronic health record system to cater for patient needs. This may include high technology systems that enable healthcare providers to critically asses the patients. The use of high levels of innovative technology reduces the chances of human era, and patients receive keen evaluation on their health condition.
Reducing Medical Errors
Reducing medical errors is a vital key quality characteristic. In order to reduce medical errors, health providers now incorporate systems that make care planning more effective by linking them to the patient’s assessment task. Computer documentation achieves timely assessment data processing for individual patients, which facilitates comprehensive information.
The computers update the patient information when the patient encounters conditional changes. For instance, patients who are in critical condition can receive automatic order support services without delays resulting from normal care planning. The computerized systems allow timely healthcare intervention when needed.
According to reports released by the National Health Institutes in America, medical errors frequently occur in the country’s clinical settings. Pressure ulcers is regarded as one of the commonly occurring medical errors. The report indicates that the rate of medical errors increased gradually from 2008-2011. According to the report statistics, one in every three American citizens experiences adverse effects that occur because of a medical error. Similarly, weekly statistics indicate that there are over forty weekly cases of wrong patient or wrong site performed surgeries. Florida health reports in 2010 indicate that almost 168 patients were harmed by medical errors that led to development of adverse effects. These errors range from wrong-site surgeries and other medical errors such as objects being left behind in the patient’s body after surgery.
Operational Definition
Patients experience wide levels of negligence in their patient care system that leads to extended hospital admissions. According to a report compiled by the Department of Health, an examination of the surgical errors committed indicated that one every ten patients died within ninety days of surgery. The deaths were reported to result from preventable medical errors. Nursing care accounted for 33% increase in the medical errors related to pressure ulcers. On the other hand, wound opening medical error increased by 6% in the year 2007-2008 (Journal of Wound, Ostomy and Continence Nursing, 2013). The use of computerized systems to monitor patients reduces the level of delay and improves service delivery.
This is one effective remedy that can be use to improve the key quality characteristics of a health center. Consequently, lack of proper patient monitoring is another common error in the management of pressure ulcers. This can lead to some complications such as development of pressure sores that occur because of lack of patient repositioning. Pressure sores make patients experience discomfort.
Therefore, using computerized systems to monitor patients can be used to reduce chances of patients developing pressure sores. In order to evaluate the importance of using the electronic health system, this essay will assess various data elements including patient demographics, medications, problems, laboratory data, past medical history and immunizations.
The type of data presented for the key quality characteristic indicator will be defined as variable data. The data collected is courtesy of the U.S National Library of medicine National Institutes of Health and the Department of Health. The data analyzed is an annual observation of the health records pertaining to medical errors from 2008-2011. The data collected represents future speculations in the health sector. The primary data sources can be found on the Risk Management Health Policy 2011 publication. The data collection methods involve an evaluation of annual health reports recorded all over the states in America. The data collected is compared against each other to measure whether there were reductions or increase in medical errors.
In order to analyze the data provided by the National Institutes of Health, this research compares random data samples from different states in the country. Further, the current baseline is a result of judgment sampling efforts. The data-sampling plan incorporates data presented from major health institutions in the country, and the baseline for the quality indicator is developed from the data analyses.
Baseline Value of the Indicator
According to the sampled data implications, the use of electronic health records has led to major improvements in the quality of healthcare service delivery. The benefit of using electronic health record systems include improved clinical outcomes, such as improved service quality and reduced medical errors. Further, the electronic systems improve organizational outcomes such as increased operational and financial outcomes. Moreover, societal outcomes are also improved. These societal outcomes include reduced costs, improved population health and improved ability to carry out research.
However, there are drawbacks associated with the use of electronic health record systems. For example, some of the drawbacks experienced are expensive maintenance costs, high acquisition costs and disruptions in the normal workflows due to the training period required in order to incorporate the new systems. Nevertheless, the benefits of using electronic health records overweigh the drawbacks of using the systems. The baseline value of using the electronic health systems is experienced in the long run. The use of electronic health systems had transformed the clinical information processing system and the level of service delivery.
There are targets and goals for using the electronic health record systems. The target of using the electronic systems is to reduce the level of medical errors that occur because of human error. Consequently, the main goal of using these systems is to increase the level of service delivery and improve the level of patient record keeping in the health sector. The goal of using electronic health systems in patient care is internally and externally developed.
The internal development entails identification of the areas that the medical errors are mostly developed. This entails internal factors such as the availability of clinical decision support tools and health information exchange within the clinical setting (Risk Management and Healthcare Policy, 2011).
On the other hand, external development of the indicator goals is realized when patients and the public explain the difficulties that they encounter in clinical operations. For instance, external development may entail ensuring there is sufficient patient satisfaction. In order to achieve sufficient levels of patient satisfaction, medical procedures such as drug information, cross-referencing patients who are allergic to a certain medication and alert for potential patient issues are processed by the electronic health systems to reduce the chances of medical error occurring (Risk Management and Healthcare Policy, 2011). The new systems are then designed to meet the external and internal goals for the healthcare system.
Descriptive Analysis of the Data
The data provided by the Department of Health simulates that the medical errors occur in most clinical settings across the country including physician offices, nursing homes, clinics, hospitals and ambulatory surgery centers. The data study shows a standard deviation of 52% represents the reimbursement claims offered to outpatients because of medical errors (Risk Management and Healthcare Policy, 2011).
The data reveals that most in-patient medical errors involve surgical errors, whereas, most outpatient errors involve late or missed patient diagnosis.
Moreover, a statistical description of international data relating to pressure ulcers shows various measures of dispersion in the medical errors. In order to evaluate the international measures of dispersion for the medical error data, we will use range to show the data dispersion among countries. The prevalence of pressure ulcers in Canada is relatively 26%, the United States prevalence to pressure ulcers is relatively 15% and relatively 12% in Jordan. However, the limitations to the measure of dispersion for the data collected occur due to different data collection methods employed by each country.
Case Study to Measure the Effectiveness of using Electronic Health Record System
In order to measure the standard deviation of pressure ulcer prevalence in a controlled area where the data has been collected evenly, we consider a research carried out by the European Pressure Ulcer Advisory Panel. The European Pressure Ulcer Advisory Panel developed a research named Pressure Ulcer Prevalence Monitoring Project to measure the level of data dispersion relating to pressure ulcers.
The data collectors for the research project were nurses with special knowledge pertaining to wound dressing. All the participants in the research survey were trained in the pressure ulcers classification and risk assessment. The total number of patients surveyed in the research was 5947 all from European countries. The report indicated that pressure ulcers prevalence was relatively 8.3% in Italy, 21-22.9% in Belgium, 12.5% in Portugal and 21% in the United Kingdom (Journal of Wound, Ostomy and Continence Nursing, 2013).
The data researched by the European Pressure Advisory Committee was assessed in Sweden using the Braden Scale and the Modified Norton Scale for the risk of pressure sores. The Swedish report indicated that use of reliable assessment tools improved the level of clinical judgment and reduced the level of medical errors committed. The Braden and Norton scales are proved to be more reliable than using nurses’ clinical judgment in evaluation of pressure ulcers prevalence risk. The Swedish risk assessment research was aimed at measuring the point of pressure ulcers prevalence, analyzing the relationship between Modified Norton Scale and the pressure ulcers prevalence and evaluating the necessary preventive measures (Journal of Wound, Ostomy and Continence Nursing, 2013).
In order to measure the quality improvement benefits associated with pressure ulcers, the Swedish government engaged in a six-stigma project to analyze the improvement variables. The six-stigma project incorporates a defining, measuring, analyzing, controlling and improvement method. The data collection setting for the six-stigma project was Skaraborg hospital located in Sweden (Journal of Wound, Ostomy and Continence Nursing, 2013).
The data was collected in one day at June 2008. The hospital provided data relating to the level of patient care services offered. The hospital has a total capacity of 460 hospital beds. The only patients excluded in the data collection were maternity patients. During the data collection day, 318 (83%) of the hospital beds were occupied. The participants in the study were voluntary and they gave their oral consent.
The six-stigma project protocol was based on a collection of the general data (hospital data), patient data, the care group data and the medical specialty data. The main goal of this project was to create an effective risk assessment plan for nurses in order to provide them with detained information about the patient skin observations. The European Pressure Ulcer Advisory Panel designed a wed-based training program for nurses to help them in their medical data collection processes.
The skin observation procedures entailed grading and localization of pressure. Pressure ulcers patients were classified according to the web based training program grading system. This included ranging patients into three categories. The first category was grade1 pressure ulcers, which include mild cases. Grade 2 represented active cases, whereas, grade 3 and 4 represented extreme cases (Journal of Wound, Ostomy and Continence Nursing, 2013).
The preventive measures for pressure ulcers were evaluated using a retrospective medical record analysis. The preventive measures entailed pressure redistribution surfaces and documented schedules for repositioning patients. A second review of the patients’ electronic health record was done 21 months after the first research was conducted. This was done to assess the level of mortality for grade 2-3 pressure ulcers cases. The Modified Norton Scale was used for risk assessment.
The modified Norton scale measured for seven variables. These variables include mental condition, food and fluid intake, mobility, physical condition, fecal contingence and general physical condition. The modified Norton scale showed good inter-rater reliability of between 0.63-0.83.
The data analysis for the research was evaluated using the statistical package for social sciences (windows version 18.0). Descriptive statistics was used to assess the patients who enrolled in the quality improvement project. The research findings proved that the use of a validated risk assessment instrument led to an effective prevention program (Journal of Wound, Ostomy and Continence Nursing, 2013).
The Effectiveness of using Electronic Health Record System in the United States
The New York Health Department is an example of the states that are committed towards using innovative data driven methods to improve the processing of health services. According to a report by the New York Health Commissioner, the city has improved its electronic health records system to 72% in 2012 (New York City Department of Health and Mental Hygiene, 2013). The New York City health department has improved medical practice based on electronic health systems to improve the general level of health surveillance by providing reliable information on the treatment, prevalence and control of health conditions in the primary setting care.
The United States of America have improved their measures designed towards improvement of their health systems to the electronic health recording systems. This was pivoted by the formulation of the Health Information Technology for Economic and Clinical Health (HITECH) act of 2009. The HITECH act involved issuing of incentives from Medicaid and Medicare to health institutions that achieve the meaningful use of the electronic health systems (New York City Department of Health and Mental Hygiene, 2013).
According to the New York City Health Department, the use of electronic health record systems improves the level of patient care quality, efficiency and safety. In addition, the uses of these electronic systems reduces the level of health disparities, improves the level of care coordination, engage the patents and their family in the treatment process and maintains security and privacy of public health information.
Emerging Issues in the Electronic Health Records Surveillance System
Leadership
There are major issues affecting the success of using electronic health records system. One of these issues is leadership. The development of an effective electronic health record surveillance system requires well-coordinated leadership structure. This is in order for the health set goals and targets to be realized. Therefore, the national and local governments in the United States work closely to foresee the implementation of effective electronic health systems. The local and state health agencies have developed a data exchange channel that enables comparable statistics to be conducted among each state.
Nevertheless, one of the challenges faced by the government in implementing electronic health surveillance systems is the conflict of priorities between the major parties involved. These parties involved include the national and local governments, electronic health records software vendors, medical providers and health information technology specialists.
Confidentiality
The establishment of a secure data sharing technology is critical because of the confidential nature of health data. The Health Insurance Portability and Accountability Act maintain that the healthcare providers exercise control on individual patient information and the release of confidential patient health information is a violation of the patient’s legal rights (New York City Department of Health and Mental Hygiene, 2013). The electronic health records are used to monitor reportable communicable diseases. In these cases, the use of identifiable patient information is necessary to prevent a disease outbreak. However, in order to use identifiable patient information, the approval by the Institutional Review Board is necessary.
Technical Issues
The developers of an electronic health record system are faced by various technical challenges. These challenges include transferring the patient information from the healthcare provider to the user who analyzes the information. Applying a uniform software standard is hard when the electronic record systems pull data from multiple electronic software platforms, which have some variations on the data storage method. The Standard and Interoperability Framework Initiative enhances private public partnerships to enable interoperability solution gaps (New York City Department of Health and Mental Hygiene, 2013).
Currently, the electronic record systems do not use a uniform standard system. This is because of the presence of many software vendors. Thus, the Standards and Interoperability Framework Initiative brings different software vendors together and test the interoperability of their software standards. Further, the initiative supports transfer of ideas among software vendors on how well to collect data from multiple sources into a single electronic records system.
Conclusion
The use of technology is procurement of health information is vital to evaluate the chances of human error in a field where errors can cost human lives. The electronic systems have boosted data collection and evaluation of data from different state health sources. The use of electronic records system can help reduce the level of medical errors reported in pressure ulcers. In addition, these systems add service value to patients who receive instant services and their previous medical histories can be easily derived. The role of electronic health records in healthcare is speculated to increase in the future after innovations continue to arise year by year.
References
Journal of Wound, Ostomy and Continence Nursing (2013). A Quality Improvement Project. Nursing Center Publications.
New York City Department of Health and Mental Hygiene (2013). Developing an Electronic Health Record-Based Population Health Surveillance System.
Risk Management and Healthcare Policy (2011). Benefits and drawbacks of electronic health record systems. DOI 10.2147/RMHP.S12985.
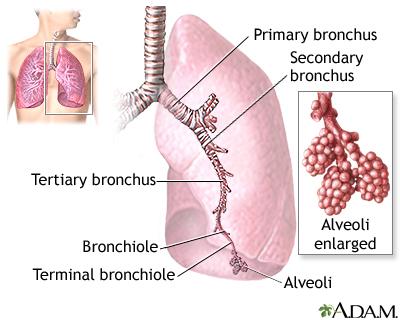 Severe Acute Respiratory Syndrome is a potential threat to societal health. This is because it can easily spread in a society. SARS is easily transmissible and severe new disease, which has emerged in this century. Communicable diseases should be handled with care to prevent severe spreading of the disease. International vaccination and disease prevention measures are designed to reduce the prevalence of communicable diseases in the community.
Severe Acute Respiratory Syndrome is a potential threat to societal health. This is because it can easily spread in a society. SARS is easily transmissible and severe new disease, which has emerged in this century. Communicable diseases should be handled with care to prevent severe spreading of the disease. International vaccination and disease prevention measures are designed to reduce the prevalence of communicable diseases in the community.
The thesis of this essay is to analyze the influences of SARS disease outbreak, analyze the epidemiological data regarding the disease, the route of transmission of the disease, analyze the international pattern of movement by individuals and how the outbreak can affect one’s community.
Severe Acute respiratory Syndrome is a lower respiratory tract disease. In the early stages of the infection, the patient develops influenza symptoms. These symptoms include fevers, rigors, myalgia, malaise and headaches. There are no symptoms proven to be specific. Thus, the infection is diagnosed with potential symptoms. The disease progresses to dry coughs, diarrhea and dyspnoea in the second week of the infection. Severe infection cases result to rapidly increasing distress in the respiratory system.
SARS was first diagnosed in an outbreak in China the year 2002. Patients in a hospital located in Tianjin, China, presented symptoms of the disease. In order to analyze the risk of SARS disease outbreak, this is evaluates the conditions of the disease during its first outbreak in China. Thus, the clinical case will provide the essential clinical characteristics of the disease and the conditions that simulate outbreak of the disease.
The China SARS outbreak in 2002-2003 was detected once haematological and physical information was obtained from the hospital’s clinical records. In order to observe the presence of the disease among patients, the percentage of neutrophillic lymphocytes and neutrophilic granulocytes were measured. Consequently, the number of white blood cells present in the patients’ blood was also measured. The hospital’s service department provided health conservation information concerning use of protective materials while handling patients. Clinicians used Fisher’s exact test to evaluate the clinical symptoms among probable and suspected SARS patients. Non-linear mixed modeling method was used to carry out tests, which were carried out to evaluate the differences between haematological patterns of suspected SARS cases and probable cases. The probable SARS patients were tested using logistic regression method to analyze the risk of death (Christian, Poutanen, Loutfy, Muller & Low, 2004).
The disease easily spread from a patient in Beijing to in-patients and healthcare workers in the hospital. The clinical situation involved 90 probable cases and 21 suspected cases reported. Moreover, 17 deaths were also reported with 15% case fatality rate. Haematological patterns were noted to be different between suspected and probable cases. The death of SARS patients who were diagnosed with probable cases was significantly linked with the most severe cases and high age. On the other hand, steroid treatment and co-morbidity showed no effect in multivariate analysis. The major effective prevention measures taken included stringent control measures. These included distribution of protective gears in huge numbers. After the last SARS patient was successfully diagnosed, protective materials were distributed at lower rates (Christian, Poutanen, Loutfy, Muller & Low, 2004).
The clinical definition of probable SARS conditions used during the China disease outbreak appeared relatively accurate in containing the condition. The disease outbreak in China showed many valuable lessons in the prevention of communicable diseases in a hospital situation. Furthermore, the situation showed the importance of readiness in terms of availability of sufficient protective gears. In addition, the situation showed how to implement preventive measures rigidly at an early epidemic stage (Serlin, 2010).
How to Prevent a SARS Outbreak
A community health nurse is a key healthcare provider who should be involved in major healthcare practices. In cases of SARS outbreak, the world health organization advises various measures to prevent wide spread of the disease within a community.
According to WHO, during a SARS outbreak, countries must be keen on the spread of the disease through immigration, and proven efficient measures should be put in place to detect and respond to SARS cases. Further, community nurses should asses keenly using epidemiological criteria in their syndromic clinical criteria. Nevertheless, efforts to prevent spread of SARS is limited to the infection’s non-specific clinical features and lack of an up to date rapid diagnostic test to detect SRAS-CoV in the disease onset. Moreover, the seasonal reoccurrence of other respiratory infections such as influenza may inhibit the surveillance for SARS. Thus, the complexity of the infection requires intensive and qualitative healthcare system implemented worldwide (Tyshenko, Paterson & Canadian Electronic Library (Firm), 2010).
SARS alert mechanism for a post disease outbreak should be done through laboratory confirmation. Consequently, the persons under investigation for SARS should be excluded from the community to prevent further spread of the disease. Thus, clinical representation, radiological and laboratory functions play a vital role in evaluation of SARS suspected cases.
In the community SARS case presented, the community nurse should incorporate the following outbreak prevention protocol. First, risk assessment assesses the community in three perspectives that include potential zone for re-emergence of SARS, nodal areas and low-risk areas. Potential zones are areas identified as major sources of previous outbreaks. Nodal areas are areas that have experienced a considerable amount of persons migrating from potential SARS prone zones. On the other hand, low risk areas are areas with no SARS history only for imported cases. After categorizing areas based on risk assessments, an SARS alert is done to increase public awareness (Tyshenko, Paterson & Canadian Electronic Library (Firm), 2010).
SARS alert objectives are to provide effective public health response, early warning of potential SARS and expedite diagnosis. SARS alert is conducted if two or more persons in a common locality fulfill the clinical definition of SARS. Consequently, after SARS alert measures are implemented, case descriptions of SARS should be accurately investigated. For instance, laboratory and radiological findings should be accurate to assist clinicians with diagnosis. In order to assess the level of person-to-person transmission the following clinical information should be evaluated. Potential exposure to SARS infection, fever of 38 degrees Celsius and over, presence of coughs, breath shortness or other breathing difficulty and chest X-rays changes resulting from SARS (Serlin, 2010).
In addition, immigration of persons from potential SARS outbreak should be assessed to prevent transmission of the infection in low risk areas. Thus, immigrants from potential SARS zones should be clinically tested for the respiratory clinical manifestations of SARS. Furthermore, a proper criterion for potential exposure is necessary in an SARS outbreak. The criteria should assess for travel made by persons from areas with SARS cases or persons who have encountered SARS suspected patients. Specific infection situations that are complex require professional intervention by the local public health unit specialists.
Air quality index is a system used to address the public about the level of air pollution. The air quality index tracks the presence of smog in the ozone and particle pollution. Air pollution is harmful to anyone in the community mostly people with respiratory diseases. Persons who exercise or work outdoors are posed to danger in cases of air pollution. Air pollution can lead to chronic and acute health effects on the community. Moreover, air pollution causes, coughing, chest discomfort, increased daily mortality and shortness of breath. People with respiratory diseases such as lung diseases and asthma are subjected to more danger. For instance, in cases where air pollution has increased, asthma patients experience worsening respiratory symptoms. This may lead to emergencies for these patients (Barrett & Stanberry, 2009).
Therefore, for people with respiratory diseases, they should reduce cumulative and short-term exposure to ozone. People with respiratory diseases can benefit majorly from exposure reductions. On the other hand, normal persons can benefit little or no benefit at all due to exposure reductions.
How an SARS Outbreak Can Affect the Community
Outbreak of infectious diseases is associated with high levels of fear in the public or communities affected. Fear is likely to be a hindrance to effective risk management of the disease and mass education mostly if the disease death levels within the community are high. Consequently, this can lead to stigma and discrimination of patients and their families. People who receive stigma are affected socially and they may delay seeking medical care or chose to stay undetected. Although the SARS 2003 outbreak did not lead to high levels of fear and stigma, Asian-American communities received some levels of isolation (Barrett & Stanberry, 2009).
The disease outbreak in China led to isolation of Asians in the United States despite their nationality or the actual risk factors for them to get the SARS disease. Therefore, it is essential for medical practitioners to identify if the community is at a great risk of experiencing discrimination, stigmatization and fear. Special attention from health professional is primal to provide immediate information regarding the disease (Ricci & Kyle, 2009).
How to modify health care practices for patients with respiratory diseases in cases of air pollution
Persons with respiratory diseases can reduce their engagement in outdoor activities at the day times when ozone levels are high. Patients can know when to avoid outdoor activities according to air quality reports and forecasts. Healthcare measures should focus on improving the level of air quality for patient with respiratory diseases. The healthcare provider can ensure patients get essential information regarding the level of air quality.
Thus, healthcare providers should assess the impact of climate change on asthma exacerbations and causation. Further, healthcare providers should also increase importance of optimal levels of indoor air quality to reduce cases of work related respiratory symptoms. Moreover, reduction in the use of nanotechnology is necessary to reduce the exposure patients to nanoparticles. Patients with respiratory infections should avoid respiratory hazards, such as isocyanates. Consequently, healthcare providers should establish a proper surveillance system for air pollution (Barrett & Stanberry, 2009).
Medical providers should apply essential knowledge concerning gene-environment interactions to increase respiratory disease prevention. Basic asthma knowledge regarding the causes of the respiratory condition can be used to develop effective prevention strategies. Personalized medicine can also be used to improve patients’ health. On the other hand, novel treatments are essential in a bid to alter the progression of respiratory disease severity. Moreover, identifying new respiratory hazards can also be used to reduce the complexity of respiratory diseases (Barrett & Stanberry, 2009).
Most governments invest costly resources in the health sector. Communicable disease poses a major challenge to the effectiveness and readiness of health sectors. The spread of SARS infection in China 2003 simulated the potential threat of communicable diseases of the society. The world health organization sensitizes that countries should ensure the proper risk assessment and management measures are well implemented. The global interactions of this century call for complex immigration cycles. These immigration cycles can lead to spread of communicable diseases through human interactions. Thus, there should be a proper global risk management protocol for communicable diseases.
The inefficiency of health systems can lead to huge loss of lives. For instance, the unpreparedness by third world African countries towards the Ebola epidemic has led to wide spread of the disease. In such situations, the safety of health staff is not guaranteed and work inefficiency due to personal fear may be encountered.
Reference
Barrett, A. D. T., & Stanberry, L. R. (2009). Vaccines for biodefense and emerging and neglected diseases. Amsterdam: Academic.
Christian, M. D., Poutanen, S. M., Loutfy, M. R., Muller, M. P., & Low, D. E. (2004). Severe acute respiratory syndrome. Clinical infectious diseases, 38(10), 1420-1427.
Serlin, D. (2010). Imagining illness: Public health and visual culture. Minneapolis, MN: University of Minnesota Press.
Tyshenko, M. G., Paterson, C., & Canadian Electronic Library (Firm). (2010). SARS unmasked: Risk communication of pandemics and influenza in Canada. Montreal [Que.: McGill-Queen's University Press.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
