+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you in High School, College, Masters, Bachelors or Ph.D and need assistance with your research paper? All you need is to ask for essay help written by a specialist in your academic field. When you buy an essay from us, we offer you an original, nil plagiarized and unique paper written by a dedicated writer who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.
Are you in High School, College, Masters, Bachelors or Ph.D and need assistance with your research paper? All you need is to ask for essay help written by a specialist in your academic field. When you buy an essay from us, we offer you an original, nil plagiarized and unique paper written by a dedicated writer who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.

Abstract
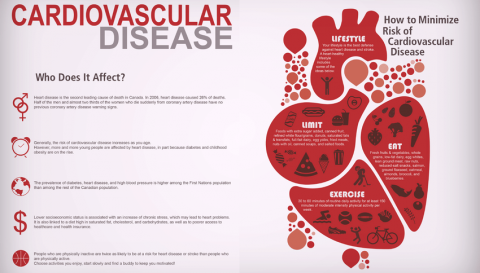 Cardiovascular diseases often referred to as C.A.D include myocardial infarction, stroke and peripheral vascular disease can be said to be the foremost reason of death in the U.S and most developed nations. It accounts for almost 900,000 deaths. Aspirin has been discovered to reduce the risks of occlusive vascular events by managing to inhibit the platelet aggregation. However, there exists differences in the way it should be administered and the patients that should get the medication. ADP has also been used in promoting the platelet function and therefore acting as an effective antithrombotic therapy. Glycoproteins are also important when it comes to the antithrombotic therapy and are used to treat coronary diseases.
Cardiovascular diseases often referred to as C.A.D include myocardial infarction, stroke and peripheral vascular disease can be said to be the foremost reason of death in the U.S and most developed nations. It accounts for almost 900,000 deaths. Aspirin has been discovered to reduce the risks of occlusive vascular events by managing to inhibit the platelet aggregation. However, there exists differences in the way it should be administered and the patients that should get the medication. ADP has also been used in promoting the platelet function and therefore acting as an effective antithrombotic therapy. Glycoproteins are also important when it comes to the antithrombotic therapy and are used to treat coronary diseases.
Introduction
For more than 100 years now, Aspirin has often been used as a pain reliever. However, since the 1970's this changed and aspiring is now being used to prevent as well as manage heart disease as well as stroke (Sixma, 2009). In fact, there is a recommendation by many doctors that people take baby aspirin for those who are risk of a heart attack (if told by their doctor) and for those persons who have been able to survive a heart attack.
The food and drug administration has come forward and argued that aspirin should be taken by the patients who have a heart disease or even a history of heart attack and stroke (Wolf et al., 2008). The FDA goes further to state that there is a risk of bleeding which sometimes outweighs the benefits of taking aspiring for the people that do not have a history of stroke or heart attack.
Acute coronary syndrome may not be classic and are often intensive; oppressive pressure on the torso that radiates widely to the left arm and abdominal pain might be an acute coronary syndrome. Further, there are other associated symptoms which include chest heaviness, burning, radiation to the neck, arms, and dyspnea. The differential diagnosis for acute coronary syndromes is extremely broad.
Doctors are often advised to treat acute coronary syndromes, this is because it is often best to err when it comes to the sides of caution and treat for an A.C.S (acute coronary syndrome) until other diagnosis. In prior times, PCI that was directly done after fibrinolytic therapy was associated with increased bleeding complications as well as reinfarction. However, this has changed with various improvements in equipment in the antithrombotic therapy (Anderson, 2009).
Cardiovascular emergencies are often life-threatening disorders which must be recognized immediately in order to avoid delay in treatment as well as minimize mortality and morbidity. The patients often have severe hypertension, cardiopulmonary arrest and in some cases chest pains. Although the benefit of aspirin is well-understood in secondary prevention, its net benefit on people without known cardiovascular diseases has not yet been established.
In fact, because of having a lower baseline risk, there is less absolute benefit from aspirin as a primary prevention for the same risk reduction (Sixma, 2009). Further, the adverse effects that are associated with aspirin appear to be completely unrelated to thrombotic risk and consequently have a lower ratio of benefit to risk for aspirin in primary as compared to secondary prevention. Although, the largest effect of aspirin is often the inhibition of thrombosis, other benefits include the increase high-sensitivity protein levels and raising the possibility of having an anti-inflammatory mechanism (Sixma, 2009).
Acute coronary syndromes include unstable angina; this might be a symptom or a change from stable angina. This angina occurs frequently occurs easily at rest, and becomes severe and lasts longer. It is noteworthy to note that although unstable angina might be relieved with oral medications it is often unstable, and it might lead to a heart attack. However, intense medical treatments and procedures are required to treat the unstable angina (Wolf et al., 2008). The Non-ST segment elevation myocardial infarction (NSTEMI) is a type of a heart attack does not cause major changes ECG. However, the chemical markers in the blood often indicate that damage and occurs to the heart muscle. In NSTEMI, and the blockage may be temporary and partial so that the extent of the damage is minimal.
ST segment elevation myocardial infarction (STEMI) is a certain type of heart attack and is often caused by a the prolonged time of blocked supply. STEMI often affects a large are of the heart muscle, and it causes changes when it comes to ECG and the different blood levels of key chemical markers (Sixma, 2009). Conversely, it is of significance to note that although some people may experience symptoms which indicate that they might soon develop an acute coronary syndrome, and others might not have symptoms until an arrest or pulmonary disease comes. Others have no symptoms of an acute coronary syndrome.
As a part of the diagnosis, there are several tests that are available. A common method is the use of an electrocardiogram often referred to as ECG, EKG, which records heart activity during rest in order to determine abnormal heart rhythms (Wolf et al., 2008). In fact, in some cases, doctors often provide heart monitors that are portable in order to record the electrical activity of the heart in a period of 24 hours. There is also the use of blood tests to measure the circulating levels of cholesterol and fats. The doctor looks at nontraditional risk factors such as the substances homocysteine, the CRP (C-reactive protein), lipoprotein and performs specific tests in order to assess the liver and kidney functions (Wolf et al, 2008).
Lastly, there is the exercise stress tests and is often known as treadmill tests, and it helps determine irregular heart rhythms during exercise. It is during the test that the heart's electrical activity of the patient is monitored through small metal sensors, and it is applied to the skin while one exercises on a treadmill (Sixma, 2009). The Aspirin has several important components, such as ant platelet/anticoagulants, they help prevent the detrimental effects of a hormone angiotensin II that constricts the various blood vessels, which reduce blood pressure and they dilate blood vessels.
The aspirin has propranolol and metoprolol and interferes with nerve receptors in the heart, and it often slows the rise of heart rate and blood pressure in exercise and stress. However, if all treatment fails and the different muscles have been damaged badly, it might require a heart transplant. The survival rate has increased for this surgery and currently stands at around 80 percent and 55% after four years.
Aspirin benefits the heart in several ways. Firstly, it decreases inflammation; inflammation can be described as a component of plaque build-up. It is this inflamed plaque that in many cases is likely to trigger a stroke or heart attack. The Aspirin often fights the inflammation that is associated with the heart disease by effectively blocking the action of an enzyme. In the instances where this enzyme is blocked, the body produces less of prostaglandins, which are chemicals as well as other functions that normally facilitate the inflammatory response (Sixma, 2009).
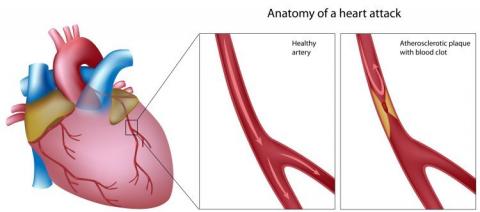
Aspirin often inhibits blood clots, the prostaglandins in the blood often trigger a series of events which cause blood platelets to clump together in order to from different blood clots (Wolf et al., 2008). Aspirin often inhibits prostaglandins and the formation of blood clots. The blood clots are often extremely harmful because when they clog the arteries supplying the heart muscle and the brain, there is an increased change of heart attack as well as stroke. Aspirin has often been able to reduce the risk of heart attack as well as be able to reduce the short term risk of death amongst the persons suffering from heart attacks (Sixma, 2009). When Aspirin is taken in the course of a heart attack, it greatly reduces the chances of heart damage and consequently increases the chance of survival.
The therapy confers conclusive net benefits in order to offer acute phase of evolving cardiovascular diseases, and it should be routinely administered to virtually every patient with a history of cardiovascular disease. A study of infarct survival more than 17,000 men and women who were suspected to have cardiovascular diseases were assigned with aspirin daily for 30 days. After five weeks, the patients that were allocated to receive aspirin had significant reductions of risk of vascular mortality (23%) nonfatal reinfarction (49%) as well as nonfatal stroke by 46%.
Further, it is of essence to note that an increase in hemorrhagic stroke as well as gastrointestinal bleeding in the patients were not seen and there was a small insignificant increase in bleeding which cannot be directly attributed to the use of aspirin. Therefore, the benefits of aspirin on risk of subsequent MI, stroke, and vascular death are substantial and the risks of serious sensitivity reactions. Therefore, the contradictions to use of aspirin when it comes to acute MI are relative, and they are not absolute.
Risks of Aspirin use
There are risks of aspirin use; evidence shows that the risk of gastrointestinal bleeding with or without aspirin often increases with age. Age and gender are often the most important factors when it comes to gastrointestinal bleeding. Research has shown other risk factors for excessive bleeding often include upper gastrointestinal tract pain, and ulcers (Berger, 2006). Nonsteroidal anti-inflammatory drug therapy which is combined with aspirin quadruples the risk for bleeding compared with the risk that aspirin alone poses.
The rate of bleeding (serious) in aspirin users can be said to be approximately two to three times greater in patients with the history of gastrointestinal ulcer. Research has shown that indeed men have twice the risk for serious bleeding as compared to women, these risk factors often increase the risk of bleeding substantially and should be considered when making the overall decision about the harms and benefits of aspirin therapy. However, the decision in regards to the exact level of risk at which all the potential benefits can be said to outweigh the potential harm that leads to gastrointestinal bleeding (Berger, 2006).
The measure of harm of the major bleeding is the leading side effect that comes with the use of aspirin. Conversely, it is of the quintessence to note that this does not include cerebral hemorrhage. This is mainly because cerebral hemorrhage is often diagnosed incorrectly in some trials. In fact, recent research has shown that cerebral hemorrhage that is caused by aspirin often reduces the benefit from treatment as compared to increasing the harm (Berger, 2006). However, it is of the essence to note that bleeding complications are not reported uniformly in all the different trials. However, the estimate of relative risk for bleeds can be said to be reliable, there is less certainty when it comes the absolute risk of bleeding complications in different control groups in several research.
It was determined that aspirin cannot be prescribed safely when it comes to primary prevention of coronary heart disease without the formal estimation of whether or not the patient has coronary disease (Berger, 2006). In fact, research has shown that the reliance of blood pressure and the use of lipids as a single factor are highly inaccurate and wrong.
The accurate risk estimation often requires the counting as well as weighting the major risks factors for coronary heart disease using risk functions that are derived from epidemiological studies such as Framingham. Therefore, it is important to understand that aspirin treatment for primary prevention should be guided using formal estimation of coronary heart disease risk using the full Framingham equation (Siegel, 2008). Research in regards to primary prevention showed that an aspirin in many cases is likely to do more good than harm.
Many people might be of the thought that avoiding myocardial infarction is of great value as compared to gastrointestinal bleeding. This group of men would in many cases decide to take aspirin in order to lower their chances of contracting a coronary heart disease risk level as compared to men who are afraid of gastrointestinal bleeding (Pignone, 2005). In fact, people who have a high likelihood of benefiting and have little potential for ham should be encouraged to use aspirin. Conversely, it is imperative to ensure that aspirin use is discouraged among men who have little potential of benefiting from the use of aspirin and have a high risk of gastrointestinal bleeding (Berger, 2006).
It is imperative to understand that the evidence on the benefits in men and women who are younger than 45 years old is often limited and the potential benefit of aspirin in this age group is low because the risk of myocardial infarction is extremely low. It has been seen that that the net benefit of aspirin often depends on the initial risks for gastrointestinal bleeding and stroke. The risk factors often include age, diabetes, smoking and history of cardiovascular disease. The excess risk of gastrointestinal bleeding that comes with aspirin, 0.7 per 1000 each year. The relative risk that exists of major gastrointestinal bleeding is 1.4, and this is completely consistent with risks that were observed in other researches.
Treatment
The optimum dose of aspirin that is used in preventing cardiovascular disease events has not yet been established. However, primary prevention trials have demonstrated the different benefits with various regimens including dosages of 100mg/d, 75mg/d and 325mg/d every other day. Further, the 75mg/d dosage is as effective as the other higher dosages. The risk of bleeding often increases with the dose (Wilson et al. 2005). Although the frequency and optimal timing of discussions that is related to aspirin therapy are currently not known, a reasonable option is that every five years in middle age and cardiovascular risk factors are detected.
The incidence of myocardial infarction and other heart diseases is often very high in older persons and, therefore, the potential benefit of aspirin is extremely large (Wilson et al. 2005). There is an established relationship between increasing age as well as gastrointestinal bleeding; therefore, the potential harms are also large. The benefit of aspirin use in persons who are older than 80 years is probably the best without risk factors for gastrointestinal bleeding.
Clinicians should be able to inform their patients about the adverse consequences that come with gastrointestinal bleeding, and the risks of taking aspirin should be explained to them (Berger, 2006). Using aspirin for the primary disease prevention of cardiovascular disease events often increases the risk for major bleeding events in both genders. In a meta-analysis, it was seen that indeed hemorrhagic strokes were higher in men as compared to women.
The indications for aspirin are divided into three categories. The first is acute treatment, and this is often used during the event, for example, taking a tablet of aspirin when one is experiencing chest pain and probably when one is in a heart attack. The second treatment use is that of primary prevention, the use of aspirin by individuals that are at increased risk of cardiovascular events but have not yet had any cardiovascular event yet (Wilson et al. 2005). This process is often important as it helps decrease the risk. Secondary prevention, on the other hand, is the use of aspirin by persons who have had cardiovascular events to reduce the risk of subsequent events. How aspirin prevents coronary diseases
Platelet adhesion, as well as activation, can be described as a part of a complex process of thrombosis which leads to vascular occlusion as well as subsequent myocardial infarctions and strokes. Therefore, aspirin is often known to be useful when it comes to cardiovascular events because of its unique inhibition of platelet aggregation that is mediated through the permanent inactivation of cyclooxygenases (Wilson et al. 2005). Therefore, blood cannot clot if one has taken aspirin and consequently this helps in greatly reducing the chance of coronary diseases. However, the underlying biological reasons for the differences that exist in terms of epidemiology and aspirin effect are not clearly understood.
Comparison with Adenosine diphosphate antagonist (ADP) and Glycoproteins with Aspirin
Adenosine diphosphate (ADP) often interacts with purinergic receptors on platelets. The initial response to ADP is often to change the shape of the platelet and convert them to a different form (Ridker, 2005). The changing of the platelet into another compound makes the blood not to clot and consequently ensures that blood does not clot in the coronary heart attack to cause a heart attack. There is, however, an important need to make sure that anti-platelet response of an individual patient is measured.
The ADP should be tailored to be given to the individual patients for the optimal effect in order to reduce thrombotic risk. ADP agents have distinct properties in the development and offers additional therapeutic options. In fact, research has shown that ADP often works well with interactions between P2Y12 receptor antagonists and natural agents which eventually contribute to the platelet function. ADP does not have side effects in terms of bleeding as compared to Aspirin. ADP has no known effects on people with gastrointestinal bleeding and it, therefore, has an advantage against Aspirin. However, the effectiveness of ADP depends on the individual as compared to Aspirin that has a high effective rate.
Glycoproteins lla/llb are important as they inhibit platelet activity of the injured coronary plaque and often focuses on the blockage of the platelet facade membrane (Ruf, 2013). The glycoproteins llb/lla binds the circulating fibrinogen, and it crosses links platelets as the common pathway to platelet aggregation. Intravenous agents are often in many cases directed towards this receptor, and it prevents platelet activity. The blockade of the platelet glycoprotein llb/lla receptor often reduces the ischemic complications, and it can be used to manage coronary infections and acute ischemic syndromes (Ruf, 2013). There is a difference in the way glycoproteins lla/llb prevents clotting with that of aspirin.
The glycoproteins lla/llb on initial contact with the platelet glycoprotein often forms a complex that binds itself to the surface preventing platelet adhesion. The fibrinogen receptor GP lla/llb is often particularly important when it comes to platelet-platelet coadhesion. Platelet adhesion and aggregation often induces intracellular signaling in Aspirin and they reinforce platelet activation, vasoconstriction and the slowing of blood flow and it increases vessel wall interactions.
The glycoproteins lla/llb does not any effect on blood flow in the heart and does not lead to bleeding as compared to aspirin. Further, the glycoproteins lla/llb has several side effects especially on men who are above eighty years old. Aspirin use is increasing in the United States and it has been argued that one can be able to use the glycoproteins lla/llb effectively in order to ensure that there is a decreased chance of coronary heart diseases.
References
Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL. (2006) Aspirin for the primary prevention of cardiovascular events in women and men: a sex- Specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
Pignone M, Earnshaw S, Tice JA, PletcherMJ (2006). Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med.
Siegel JE,Weinstein MC, Russell LB, Gold MR (2008). Recommendations for reporting Cost-Effectiveness analyses. Panel on Cost-Effectiveness in Health and Medicine.JAMA.;276:1339-1341.
Anderson KM, Odell PM, Wilson PW, Kannel WB (2009). Cardiovascular disease risk profiles. Am Heart J.
Murphy M, Foster C, Sudlow C, et al. (2005) Cardiovascular disorders: primary prevention.Clin Evid. June:91-123.
Wolff T, Miller T, Ko S. (2009) Aspirin for the primary prevention of cardiovascular events: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern
Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL. (2006) Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta- analysis of randomized controlled trials. JAMA.; 295:306-13.
Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al. (2006); American Heart Association Statistics Committee and Stroke Statistics Sub-committee. Heart disease and stroke statistics—2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation.113:e85-151.
Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, et al. (2005) randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med.;352:1293-304.
Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB (2008). Probability of stroke: a risk profile from the Framingham Study. Stroke. SAGE.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (2005). Prediction of coronary heart disease using risk factor categories. Circulation.;97:1837-47.
Sixma JJ (2009). Interaction of blood platelets with the vessel wall. In: Bloom A, Forbes CD, eds. Haemostasis and Thrombosis. 3rd ed. New York, NY: Churchill Livingstone:259–285.
Ruf A, Patscheke H (2013). Platelet-induced neutrophil activation: platelet-expressed fibrinogen induces the oxidative bursts in neutrophils by an interaction with CD11c/CD18. Br J Hematol. 21:119–122.
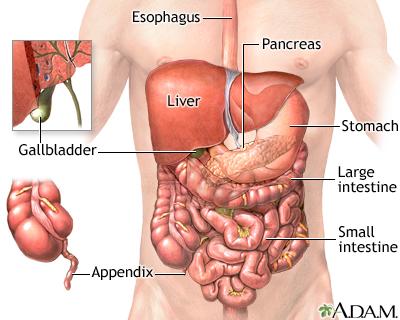 Abdominal pains may be caused by a number of serious underlying illnesses that can be diagnosed and treated. The occurrence of abdominal pains may also be caused by common illnesses such as indigestion, food allergies or even appendicitis (Golan & Tashjian, 2012) .
Abdominal pains may be caused by a number of serious underlying illnesses that can be diagnosed and treated. The occurrence of abdominal pains may also be caused by common illnesses such as indigestion, food allergies or even appendicitis (Golan & Tashjian, 2012) .
Test done for the 13 year old female patient may be expected to reflect suspected illness. It would be important to first test for the presence of any infectious agents that may have caused the abdominal pains. The infectious agents may be the rotavirus which is a common virus that affects children to cause symptoms that include abdominal pains (Golan & Tashjian, 2012). Therefore, it would be important not to overlook the possibilities of microbial infection. The suggested treatment for this condition would be use antibiotics and dietary change (Golan & Tashjian, 2012).
Another reason that may cause the abdominal pains may be chronic functional abdominal pain (CFAP). This condition may be present when tests do not show the occurrence of any infection. Functional abdominal pain is caused by a disorder in the transmission of pain impulses. This occurs by action of magnification of the stimulation of the nociceptive impulses from the gastrointestinal tract (Golan & Tashjian, 2012). The cause of this illness may be due to various reasons. Since this condition is not entirely associated with the gastrointestinal tract, it would occur due to a bio psychological disorder (Golan & Tashjian, 2012) . The symptoms of CFAP may also arise due to traumatic life experiences such as sexual abuse or loss of loved ones (Buttarp, Trybulski, Polgar, Sandberg-cook, 2013). It may be due to the fact that emotions may stimulate nociceptive receptors related to the gastrointestinal tract. The treatment for this condition would involve cognitive behavioral therapy which may help in the elimination of thoughts that may trigger the pain. Use of antidepressants is also important as the also act as pain relievers in the abdominal area.
Another cause of the abdominal pain may be the occurrence of dysmenorrhea. It should not be ruled out since the female patient has is old enough to experience menses. Dysmenorrhea is simply painful menstruation (Buttarp, Trybulski, Polgar, Sandberg-cook, 2013). Dysmenorrhea may be caused by production of too many prostaglandins that may cause contraction of the myometrium which in turn may result in pain (Golan & Tashjian, 2012). The most likely dysmenorrhea expected would be primary dysmenorrhea. The management of this condition would involve the use of non-steroidal anti-inflammatory drugs. The drugs include Ibuprofen, Meclofenamate or Naproxen.
Another cause of the abdominal pain may be the occurrence of recurrent abdominal pain which mostly occurs during childhood (Buttarp, Trybulski, Polgar, Sandberg-cook, 2013) . psychological distress may cause abdominal pain symptoms. It can be managed by cognitive behavioral therapy. Recurrent abdominal pain may also be caused by an infection due to presence Helicobacter pylori which can be easily managed by use of antibiotics (Buttarp, Trybulski, Polgar, Sandberg-cook, 2013).
It would also be important to take a pelvic exam because the abdominal pain may be caused by a history of pelvic fracture that may cause stimulation of pain. Urine analysis may also be recommended to test for an occurrence of kidney stones which cause symptoms which include abdominal pain (Golan & Tashjian, 2012). Endoscopy would be recommended when there is suspicion of a problem with organs in the gastrointestinal organs which would be done by a gastroenterologist (Buttarp, Trybulski, Polgar, Sandberg-cook, 2013). If the tests would suggest the occurrence of recurrent abdominal pain it would be important to refer the patient to a pediatrician who would do further tests to ascertain the diagnosis.
References
Buttarp, M., Trybulski,J., Polgar, B, P., Sandberg-cook, J., (2013). Primary Care. Elsevier Health Science Division ISBN: 9780323075015.
Golan, D. E., & Tashjian, A. H. (2012). Principles of pharmacology: The pathophysiologic basis of drug therapy. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
1.1. Definition and overview of acute coronary syndrome
 In medicine, acute coronary syndrome refers to conditions in the human blood that result from inadequate blood supply in the heart. A couple of disorders contribute to the generalized term of the syndrome in the human body (In Fang, 2011). Diagnosis of acute coronary syndrome is possible if timely. Often emergency rooms in hospitals are the common channels for diagnosis of the syndrome (Jackson, 2008). Apparently, the method of treatment adopted by a doctor on the patient is dependent on certain varying factors on the nature of the coronary syndrome. Signs, symptom, and the general body health are some of the common determining factors towards the method of treatment used on patients suffering from the disorder (Bhagavan, 2011).
In medicine, acute coronary syndrome refers to conditions in the human blood that result from inadequate blood supply in the heart. A couple of disorders contribute to the generalized term of the syndrome in the human body (In Fang, 2011). Diagnosis of acute coronary syndrome is possible if timely. Often emergency rooms in hospitals are the common channels for diagnosis of the syndrome (Jackson, 2008). Apparently, the method of treatment adopted by a doctor on the patient is dependent on certain varying factors on the nature of the coronary syndrome. Signs, symptom, and the general body health are some of the common determining factors towards the method of treatment used on patients suffering from the disorder (Bhagavan, 2011).
Over the past decade, treatment of coronary syndromes posed severe challenges to doctors and often contributed to death of many patients suffering from these disorders. In United States, the disorders are the highest contributor towards death cases reported in the country (Pablo, 2014). Apparently, casualties from the disorder have a high variance from other disorders. However, in the last decade, the trend in the number of deaths reported caused by the fatal disorder is decreasing at a high rate (Lehne, 2013). The rapid decrease of death cases from acute heart disorders attributes to the rapid responses to the disorder and the global campaign against the disorder. Global campaign against acute coronary disorder has a high reliance on the advancement of the drugs used during the treatment process (Bhagavan, 2011). Apparently, some measures and drugs used such as statins and anticoagulation are some of the milestones made by drug researchers towards the global concern (Papadakis, 2013).
1.2. Objectives
The paper reviews the in-depth use of anticoagulant while managing coronary disorders. It makes a comprehensive analysis on the different types of anticoagulant through an all-inclusive analysis by comparing and contrasting their benefits while responding to the global concern (Pablo, 2014). Additionally, the paper objects at providing an evidence-based of the agents focusing on their effectiveness while treating, reducing the death rates among the patients and as well, the possible post-exposure side effects to the patients (Lehne, 2013).
2.Clinical explanation of Acute Coronary Syndromes
2.1. ACS pathophysiology
Before highlighting on the treatment methods used while responding to the disorder in patients, it is essential having a clinical understanding of the disorder in patients. Pathophysiological approach towards ACS is essential as it enhances understanding of anticoagulants (In Ferro, 2013). As highlighted earlier, ACS results from inadequate blood in the heart. Often, insufficient blood levels in the heart may result from buildups of plaques in the arteries supplying blood to the heart (Clark, 2010). Apparently, plaques in arteries arise due to fat deposition in the artery walls that contribute to narrowing of the blood vessels. Surprisingly, unlike in most cases where narrowing of vessels contributes to an increased pressure, often, narrowed arteries increase the difficulty experienced by blood flowing in the arteries (In Fang, 2011).
In the human body, blood plays a great role of distributing oxygen and nutrients to different body parts. Conversely, reduced blood flow in the vessels contributes to insufficiency of oxygen pumped to these parts. The situation is risky as it may lead to periods of heart attacks and as well, chest pains on the patients. In most cases, mostly reported on patients suffering from the syndrome, the disorder attributes to the rupturing of the plaques that leads to the development of clots in the vessels (Herzog, 2009). Similarly, blood clots and plaques in the vessels concurrently increases the difficulty experienced by blood as it flows in the body. In cases where there is a drastic reduction of blood flow to heart muscles, chances of occurrence of heart attacks increases (In Ferro, 2013).
2.2. Types of ACS
Several types of ACS exists based on the causative agents and intermediate symptoms. Common types include:
a. Unstable Angina
It is an abnormality in the cardiac system caused by existence of blood clots in the blood vessels. Clots as seen earlier contributes to blockage of vessels directing blood into and out of the heart thus leading to reduced blood flow (Clark, 2010). Unstable angina differentiates from other types in the human body due to its conservative effects that do not lead to overall damage of heart muscles. Intermediate symptoms experienced by patients with the condition include discomforts due to chest pains (In Fang, 2011).
b. heart attack
Unlike the unstable angina, heart attack attributes to damage of the heart leading to its malfunctioning. Apparently, it originates from blocked coronary vessel leading to damage of heart muscles (Papadakis, 2013).
c. Myocardial ischemia
It is the last type of ACS in the discussion and attributes to restriction of blood flow in tissues leading to the shortage of vital nutrients and oxygen. Normally, reduced blood flow originates from partial or full blockage of heart arteries. Conversely, supply of oxygen reduces leading to the reduction of the heart’s ability of pumping blood effectively to other body parts (Lehne, 2013).
2.3. Symptoms of ACS
Based on the earlier discussion, the basic symptom is chest discomforts. Patients suffering from unstable angina mostly experience pain resembling heavy pressures on the chest (Clark, 2010). Similarly, pain may increase based on the degree of risk posed by the disorder. Severe risks contribute to pain on the left side of the body. On the other hand, in diabetic patients, they experience exemplary symptoms such as vomiting, light headaches and sweating (Papadakis, 2013).
2.4. Causes and Risk factors to ACS
Most of the ACS cases arise from narrowing of heart arteries. Narrowing is due to the existence of fats on the artery walls (Herzog, 2009). Similarly, inflammation of heart arteries and blood clots also leads to the disorder. On the other hand, common risk factors linked with ACS include; past history of high blood pressure in patients, high cholesterol diet intake, family history on prevalence of the disorder and individual inactivity that leads to deposition of fats on these walls (In Ferro, 2013).
2.5. Diagnosis process of ACS
Sometimes it is challenging for doctors while distinguishing ACS and other disorders leading to chest pains (Clark, 2010). However, over interventions from different campaigns on the human heart health led to the development of two tests done on patients. Occasionally, the differential diagnosis process of ACS is broad. During the diagnosis process, it is essentially considering pulmonary embolism and aortic dissection cases since they are life threatening to patients (Pablo, 2014). Similarly, their treatment is different while compared to ACS. Major diagnosis processes involve tests. Two major tests carried out on patients presenting symptoms of ACS include:
- Electrocardiograph (ECG)
It is a heart-tracing test aimed at determining abnormalities in heart pattern tracing. Prevalence of ACS presents abnormal traces (Herzog, 2009). Pathologists carry out the test on their patients occasionally focused at evaluating the general rhythm of the heart patterns. The test is important while controlling the prevalence of ACS in patients as it gives valuable information on the location and the degree of prevalence of the dead tissues in the heart. In addition, the test is valuable while differentiating ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI).
- Blood tests
A chemical-based test that measures troponin in a blood sample. Troponin is a chemical substance found in the heart muscles (Laposata, 2011). Among pathologists, damaged heart increases probabilities of releasing the chemical to the bloodstream. Conversely, it is a suitable indicator of heart attack in patients with chest pains. Under normal situations, the levels of the chemical start rising on the onset of chest pains in the patient. However, these levels elevates as the patients subjects to chest pains and can last up to 14 days.
Blood tests, also called biomarkers, is valuable while determining cases of NSTEMI. Apparently, unlike in STEMI cases where biomarkers do not offer opportunities of reperfusion, NSTEMI biomarkers indicate high levels of sensitivity (Clark, 2010). Therefore, it is possible for pathologists to identify patients at great risks (In Dardenay, 2014).
3. Treatment of ACS
As in other disorders faced, there are several available treatment procedures. Common procedures include drug prescription. These drugs have components that aid in eliminating the clots and fats in the arteries (In Dardenay, 2014). Furthermore, treatment differs depending on the nature of ACS suffered by the patient. Similarly, timely treatment relies on the risk score of the patient. Major treatment methods used include;
3.1.1. Fibrinolysis therapy
It is the immediate standard of management of STEMI. While using fibrinolysis, the ultimate goal is the removal of myocardial necrosis wave front while saving a threatened myocardium and thus improving the patient’s survival. Apparently, according to factual statistics presented on the effectiveness of the therapy, fibrinolysis reduces death rates on patients with ACS by 30%. (Hong, 2008)
3.1.2. Limitation of fibrinolysis therapy
The treatment procedure adopted while dealing with elevated ST segment is selective and does not benefit all patients presenting STEMI cases. Often, ST depression and T inversion do not benefit from the therapy (Laposata, 2011). Additionally, while using the therapy on patients, patients increase their risks of intracranial hemorrhage, which is a complication that leads to death. Lastly, while using the therapy, patients are prone of suffering from uncontrollable blood pressures resulting from intracranial hemorrhage (In Dardenay, 2014).
3.2. Antithrombotic therapies
These are therapies aimed at reducing clots in blood vessels. Drugs used in the therapy mostly aim at manipulating platelet activity in the blood. Common antithrombotic include:
3.2.1. Aspirin
Based on ACS mortality rate records, after introduction of aspirin on patients with ACS, death rates reduced drastically (Lehne, 2013). In comparison to earlier used drugs such as placebo, aspirin increases survival of patients and thus the recommendation of giving patients with STEMI aspirin daily. However, aspirin presents allergic reactions on patients thus increasing its limitation on the users (Clark, 2010). Despite the recommendation of daily dosage of aspirin, increased dosage of above 100 mg daily does not present advantages to patients thus limiting the dosage to 100 mg (Laposata, 2011).
3.2.2. Adenosine Diphosphate (ADP)
The most common used ADP is the clopidogrel. Research carried out with 12000 patients presenting NSTEMI resulted to the reduction of the intermediate symptoms and death chances by 20%. More so, combination of the dosage with aspirin indicated a benefit to STEMI. It contributed to reduction of the mortality rate among the patients. It is another vital dosage to patients with NSTEMI (Hong, 2008). Similarly, like aspirin, high dosages above 600 mg do not have additional benefits to patients and thus not advocated by pathologists. Another important limitation of the drug is the complex processes involved during its metabolism. Unlike other forms of drugs used while dealing with common disorders experienced, clopidogrel exists in its inactive form and body enzymes and tissues converts it to its active form to enhance its effectiveness in the body (Mandell, 2011).
3.2.3. Ticagrelor and prasugrel
These drugs exist as alternatives to clopidogrel. They are essential while controlling ACs conditions attributing to blood clots in the arteries. Unlike the later, these alternatives have high activity rates in the body and are less variable in patients (Hong, 2008). Their activities while in the blood is faster while compared to the overall effectiveness of clopidogrel. Trial of the drug’s effectiveness on patients revealed their significance while substituting clopidogrel. Results from the samples presented reduced death rates of ACS patients. However, the study as well presented a limitation of these drugs on patients with histories of stroke and heart attacks. These patients presented high risks of bleeding while diagnosed with the alternatives unlike while diagnosed with clopidogrel (Laposata, 2011).
3.2.4. Glycoprotein IIb/IIIa antagonists
Unlike in the past years, continued use and reliance of these dosages while responding to ACS cases is drastically reducing. Apparently, the reduced use of these drugs attributes to the routine pretreatment of ACS using thienopyridines. In most cases, these antagonist drugs are essential when there is no routine antiplatelet and as well when a patient with ACS has a prescription of heparin (Brenner, 2012). In a study survey using the prescription of the drug, results revealed high reduction of cardiac complications in patients with STEMI. Similarly, among patients with NSTEMI, high risk reduced drastically when the patients began their dosages of the drug. GP IIb/IIIa inhibitor are essential drugs in the management of acute coronary syndromes in high-risk cases. Furthermore, pathologists use these drugs as alternatives to aspirin and ADP inhibitors (Mandell, 2011).
3.2.5. Beta-blockers
They are additional anticoagulant agents used while treating cases of STEMI in patients. Unlike in the past, before trials on the generalized effectiveness of the drug on patients, currently, the drugs is as well playing part while managing NSTEMI. Administration of the drug to patients is through both oral and intravenous metoprolol (Laposata, 2011).
Studies on the beta-blockers in the modern society revealed that early use of the drug on patients raises their risks. Mouth metoprolol used on patients contributed to a massive reduction of the reinfarction and fibrillation of the heart ventricles (Mandell, 2011). However, it increases the risks of patients of getting cardiogenic shocks. Conversely, the mortality rate of early offsets did not reduce. Henceforth, it contributed a decline in early use rates of beta-blockers. More so, due to the alarming death rates, standard care made shifts from beta-blockers to other anticoagulant agents (Lehne, 2013). Additional limitation and health risk threats posed by the agent to patients included cases of heart failure and low blood pressure among the elderly. Lastly, despite the agent aimed at increasing the survival of patients, it, on the other hand, lead to additional health issues when used in early offset of ACS. However, among patients presented late to the drug, they as well have larger risks of developing coronary complications. Mostly, pathologists make prescriptions to their patients on not ultimately discharging their patients under beta-blocker therapy after a heart failure case as it may increase the risk of future health complications if rushed on starting the prescription early (Mandell, 2011).
Nevertheless, despite the drawbacks of the drug highlighted in the discussion above, in patients recovering from cardiac arrest but experiencing seasons of ventricular dysfunctions, Capricorn, a beta-blocker, may have significant advantages to the patients as it reduces their death rates and reinfarction. Thus, Capricorn becomes the preferable beta-blocker in patients with STEMI (Bhagavan, 2011).
3.2.6. Angiotensin-converting enzyme inhibitors
It is another significant anticoagulant agent used on patients recovering from heart failures. Studies on patients presenting symptoms of ACS indicated a reduction of mortality rates of patients after subjection to these enzyme inhibitors. Precisely, patients with ejection fraction are the highest beneficiaries from the dose (Brenner, 2012). While making prescription of patients with the ACS, major considerations made include; the type of ventricular dysfunction where left is the most considerable and the number of days after MI where pathologists commend the first 30 days (Mandell, 2011).
Wrong timing while using the drug has severe risky outcomes on patients. In a study investigating the impact of early offsets of the anticoagulant agent on ACS patients, it revealed that early starts encounter premature stops due to the worse outcomes such as heart attacks. Similarly, the study revealed need of using the dose on stabilized conditions of patients. Unstable ACS, when treated with the enzyme inhibitors, lead to severe cardiac complications (Laposata, 2011).
3.2.7. Intensive statin therapy
Statins have beneficial roles on secondary prevention on ACS victims. Research on the effectiveness of the drug while managing the prevalence of ACS revealed that the high dosage of the drug has high positive outcomes as compared to low dosages (Brenner, 2012). Aiming at supporting the difference in the outcomes, a study aimed at investigating the overall effectiveness of statins revealed that high dosages of intensive statins have low rates of cardiac complications where these outcomes persist for periods of over 30 months in the patients (In Dardenay, 2014). Unlike the other anticoagulant agents used on ACS victims, intensive statin therapy has consistent outcomes regardless of the risk conditions of patients. Apparently, high dosages of the drug did not have considerations of the patient’s state, which present either stable or unstable ACS. Currently, pathologists are making recommendations to their patients on reliance on high dosages over low dosages of statins (In Fang, 2011).
3.3. Factors influencing the anticoagulant agent used on ACS patients
As seen earlier in the discussion on the treatment procedures used in the management process of ACS, it is clear on the existence of a couple of agents used as alternatives. The discussion below anticipates developing a comprehensive analysis of the factors influencing the choice of anticoagulant agent (Laposata, 2011).
Allergy. It results from the reaction between antigens and antibodies in the body. Allergy has severe effects on individuals as it may contribute to increased mortality risks based on the nature of antigens. Aspirin allergic patients cannot rely on an aspirin dosage due to the chemical components used in the manufacture of the drug. Conversely, allergy limits the use of aspirin as an anticoagulant in patients (Bhagavan, 2011).
Nature of ACS. STEMI, NSTEMI, and as well attributed symptoms such as ventricular dysfunctions influence the nature of treatment procedure used in patients. Left ventricular dysfunction cases in patients calls for angiotensin-converting enzyme inhibitor as the immediate treatment method used. Therefore, the type of ACS influences the nature of anticoagulant agent used (In Fang, 2011).
ACS offsets. These factors influence the recommended period of administration of drug dosages in patients. Some anticoagulant agents have differentiable outcomes when administered at different stages of recovery from MI. Early stages of beta-blockers lead to increased risks of cardiac complications. Hence, in cases where there is a need of early offsets of agents, beta-blockers are not preferable. In addition, the timespan while recovering from MI influences the nature of agents used (Laposata, 2011). While using angiotensin-converting enzyme inhibitor, pathologists make recommendations of using the dosage during the first 30 days of recovery.
4. Conclusion
In conclusion, ACS is a fatal condition facing many people globally. Early management of the disorder is essential as it reduces the mortality rate (Jackson, 2008). The condition attributes to reduced blood flow caused by narrowness of heart arteries due to deposition of fats and blood clots. While managing the condition in patients, anticoagulant agents play essential roles in controlling the narrowness level of these arteries by manipulating the fats and clotting effects of platelets. Commonly used anticoagulant agents used include; aspirin, which reduces the sticking effect of platelets in the blood and beta-blocker drugs that reduce the heart rate on patients presenting abnormalities in the heart rhythm. Additionally, statins, which lower the fat level in the blood vessels and ACE inhibitors (responsible for protecting the heart) aid in managing the prevalence of the condition among patients. During the management process, timely diagnosis is crucial as it reduces heart complications and rise of risky health conditions in patients. Apparently, while recovering from ACS, pathologists often make recommendations on their patients to ensure they maintain the right tracks by avoiding risk factors while avoiding health complications (Jackson, 2008).
References
Laposata, M. (2011). Coagulation disorders: Quality in laboratory diagnosis. New York: Demos Medical Pub.
In Fang, M. C. (2011). Inpatient anticoagulation.
Bhagavan, N. V., & Ha, C.-E. (2011). Essentials of medical biochemistry: With clinical cases. Amsterdam [etc.: Elsevier Academic Press.
Lehne, R. A. (2013). Pharmacology for nursing care. St. Louis, Mo: Elsevier/Saunders.
Brenner, G. M., & Stevens, C. W. (2013). Pharmacology. Philadelphia, PA: Saunders/Elsevier.
Papadakis, M. A., & McPhee, S. J. (2013). Quick medical diagnosis & treatment.
In Ferro, A., & In Garcia, D. A. (2013). Antiplatelet and anticoagulation therapy.
Mandell, J. E. (2011). Ventricular fibrillation and acute coronary syndrome. Hauppauge, N.Y: Nova Science.
Hong, M. K., & Herzog, E. (2008). Acute coronary syndrome: Multidisciplinary and pathway-based approach. London: Springer.
Herzog, E., & Chaudhry, F. (2009). Echocardiography in acute coronary syndrome: Diagnosis, treatment and prevention. London: Springer.
Clark, D. S., & American Academy of Family Physicians. (2010). Acute coronary syndrome. Leawood, KS: American Academy of Family Physicians. Kasliwal, R. R. (2009). Acute coronary syndrome. Haryana, India: Elsevier.
Jackson, G. (2008). Acute coronary syndromes. Oxford: Oxford University Press.
Pablo, A. (2014). Pharmacological Treatment of Acute Coronary Syndromes. Springer London.
In Dardenay, E., & In Cocheret, C. (2014). Acute coronary syndrome: Symptoms, treatment and prevention.
Congestive heart failure is a disease that affects the heart’s ability to pump enough blood. Therefore, the disease leads to a decrease in the cardiac output. This causes shortage in the supply of oxygen and nutrients to body organs. Various factors lead to the congestive heart failure condition. These factors include fatigue, swelling or edema, shortness of breath and diminished exercise capacity.
The diagnosis of the congestive heart failure is achieved by various observations. These observations include the individual’s medical history, selected laboratory tests and a keen physical examination.
Patient’s Physical Examination
In order to evaluate if the condition presented is congestive heart failure, the medical practitioner should carry out a physical examination on the patient. During the physical examination, the physician examines the underlying cause of the condition, after assessing the level of heart functioning. Physicians use stethoscopes to assess whether heart sounds are normal. Abnormal heart sounds indicate a barrowed or leaky valve. Further, the stethoscope enables the physician observe whether there is fluid accumulation in the lungs. Moreover, the physician also examines if the patient has enlarged veins present in the neck and if the patient has swellings in the legs or abdomen (Dains, Baumann & Scheibel, 2007).
Patient History
Furthermore, while evaluating a patient presenting with congestive heart failure, it is vital to assess the patient’s previous medical history. This includes information about drug or substance abuse, history of hypertension, prior heart attack or chest pains, recent pregnancy or recent viral illness. These observations help the physician make some key conclusions about the patient’s condition. For instance, the disease may occur because of a previous medical condition such has heart attack (Dains, Baumann & Scheibel, 2007).
Diagnostic Tests
Diagnostic tests mainly include use of an electrocardiogram, echocardiogram and cardiac catheterization. These tests help the physician evaluate the level of heart functioning and detect heart malfunctions. These heart malfunctions include coronary artery disease, valve dysfunction and heart attack. An electrocardiogram test is used to measure the level of electrical activity in the heart. The test is done by connecting electrical sensors (leads) attached to predetermined positions in the chest, arms and legs. These electrical sensors (leads) record electrical activity and they help evaluate the level of heart functioning.
On the other hand, an Echocardiogram is an ultrasound assessment of the heart that produces detailed images of the heart. This is done to detect abnormal conditions present in the heart structure and to measure the extent of ejection fraction. Patients with low ejection fractions display severely depressed heart functioning. Further, cardiac catheterization entails injecting a small amount of a radioactive dye into the left ventricle. This is done through a catheter, which is a long flexible tube. The catheter has a special camera that evaluates how much of the radioactive dye is ejected from the heart after each heart beat. Cardiac catheterization is mostly performed on patients with angina and patients who have a medical history of heart attacks. This test is mostly done to determine whether the heart failure is caused by coronary heart disease (Seller & Symons, 2012).
In some cases, stress tests are also used to examine the possibility of coronary artery disease. there are various types of stress tests. For instance, a patient may be simply asked to walk on a treadmill while connected to an electrocardiogram. In other cases, a drug is infused into the blood stream to increase the heart rate or to trigger the flow of blood within the heart. An electrocardiogram is used to capture heart images for further observations.
These tests enable the physician assess whether the condition presented is congestive heart failure or another heart condition. Moreover, if physical symptoms indicate the presence of congestive heart disease, these tests are used to confirm the observation (Goolsby & Grubbs, 2011).
Question 2
Before choosing a final diagnosis a clinical observation criteria must be followed. This criteria entails collecting all relevant clinical history about the patient presenting with pharyngitis (sore throat). The clinical history of the patient entails recent exposure to people with pharyngitis, previous medications (allergic reactions), presence of allergies or intolerances by the patient and previous complains about the condition (Jill, Cash & Glass, 2010).
If the previous complaints are frequent, the pharyngitis condition may be caused by another condition such as aphthous ulcers. Further, the clinical observation should also evaluate the patient’s recent travel history. This information may help is examining the location and setting of the patient that may lead to arthropod exposure (Goolsby & Grubbs, 2011). In addition, this may enable the physician examine if there is possibility of pre-travel vaccination or other prophylactic medications consumed by the patient.
Further, clinical examination findings are another major clinical observation that are used to determine the final diagnosis. This includes examination of the patient’s constitutional features such as headaches, anorexia, muscle pain, fatigue or malaise. Consequently, there should be a throat examination to evaluate the severity of the sore throat pain. Throat observations are also necessary to determine if the sore throat is caused by ulcerations, uvular oedema or tonsillar enlargement (Bickley, 2010). Drug and substance abuse may also be a disposing factor for the throat condition.
Some of these clinical presentations are essential because they are used to indicate whether there is need for additional diagnostic tests. For instance, patients with severe symptoms such as drooling, difficulty in swallowing, asymmetrical appearance of the pharynx or tonsils and significant neck swellings may indicate the presence of other infections. Thus, a plain radiograph may be used to assess the level of soft tissue swelling. In case the situation is critical, the physician will require a contrast enhanced computer axial tomography scan. This scan helps to define the anatomy of the condition (Dains, Baumann & Scheibel, 2007).
Therefore, criteria of clinical observations are necessary to evaluate the final diagnosis. Sore throats are common, and they affect individuals from all age groups. However, the disease is common among children and young adults. The final observation of sore throat infection should be pre-determined by medical observations. This is because upper respiratory diseases or bacterial infections in younger patients may cause sore throats. Sore throat complaints may also require physical observations of the oral cavity, neck, larynx, oropharynx and thyroid gland. This is because diseases in the oesophagus, heart or stomach sometimes may cause the pain experienced in the throat (Bickley, 2011).
In order to determine the final diagnosis for a patient presenting with sore throats, clinical observations should be accurate in determining the cause of the infection. This is necessary in order to achieve patient-centered care, which is effective in the treatment of most diseases. Further, criteria of clinical observations may detect other malfunctions that were not reported by the patient.
References
Dains, J. E., Baumann, L. C., & Scheibel, P. (2007). Advanced health assessment and clinical diagnosis in primary care. St. Louis, Mo: Elsevier Mosby.
Lynn S. Bickley. (2010). Guide to Physical Examination and History Taking. Lippincott Willians & Wilkins, ISBN: 9781609137625.
Lynn S. Bickley. (2009). Bates’ Pocket to Physical Examination and History Taking. Lippincott Williams & Wilkins, ISBN: 9781451173222.
Mary Jo Goolsby; Laurie Grubbs. (2011). Advanced Assessment. F.A Davis Company, ISBN: 9780803621725.
Jill C. Cash, Cheryl A. Glass. (2010). Family Practice Guidelines. Springer Publishing Company, Incorporated. ISBN: 9780826197825.
Seller, R. H., & Symons, A. B. (2012). Differential diagnosis of common complaints. Philadelphia, PA: Elsevier/Saunders.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
