+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help in your homework? All you need is to ask for research paper help written by a specialist in your academic field. When you buy an essay online from My Essay Services, we offer you an original, nil plagiarized and unique paper written by a dedicated writer who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.
Are you in High School, College, Masters, Bachelors or Ph.D and need someone to help in your homework? All you need is to ask for research paper help written by a specialist in your academic field. When you buy an essay online from My Essay Services, we offer you an original, nil plagiarized and unique paper written by a dedicated writer who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.

Question 1
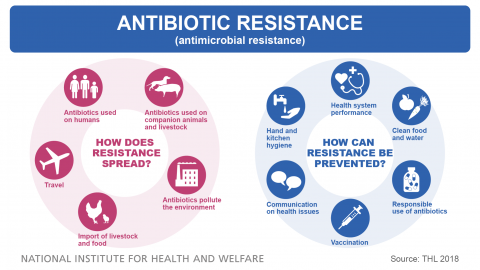
 Broad-spectrum antibiotics are used in the treatment of a wider range of diseases caused by bacteria. They are appropriate in use when the physician is unable to identify the bacteria that caused the infection. Broad spectrum antibiotics, therefore, can act on both gram positive and gram negative bacteria. They find application in situations when there is super-infection, a condition when the disease is caused by different types of bacteria (Anderson, 2012). Such situation warrants administering of broad-spectrum antibiotics or a combination of the antibiotic therapy. The clinician can administer the broad spectrum antibiotic when there is drug resistant bacteria that does not respond to narrow spectrum antibiotics.
Broad-spectrum antibiotics are used in the treatment of a wider range of diseases caused by bacteria. They are appropriate in use when the physician is unable to identify the bacteria that caused the infection. Broad spectrum antibiotics, therefore, can act on both gram positive and gram negative bacteria. They find application in situations when there is super-infection, a condition when the disease is caused by different types of bacteria (Anderson, 2012). Such situation warrants administering of broad-spectrum antibiotics or a combination of the antibiotic therapy. The clinician can administer the broad spectrum antibiotic when there is drug resistant bacteria that does not respond to narrow spectrum antibiotics.
It is inappropriate to administer broad spectrum antibiotics for relieving cough, cold and flu symptoms. Broad-spectrum antibiotics are readily available even as over the counter medicine, a worrying situation that could lead to drug resistance (Anderson, 2012). Development of multidrug-resistant strains of the bacteria places the risk not only at the community level but also at the globe. This is due to the fact that bacteria spread quickly, and their infective rate is also high. Such resistant strains pose a problem especially in the hospitalization costs and research. Furthermore, most of colds and flu are caused by influenza viruses (Edmunds & Mayhew, 2013). It would be ineffective to treat virus diseases with antibiotics since most of the viral infections are managed by immunization.
Common cold and flu keep most people away from jobs and even school. The symptoms associated with the common cold make individuals seek medical attention. Symptomatic treatment is the best approach against the common cold (Edmunds & Mayhew, 2013). The symptoms of flu or the common cold include headache, congestion, muscle ache, fever, and lacrimation among others. Some of the symptoms can be managed by administering painkillers, zinc supplements and decongestants. The health practitioner may recommend close monitoring in situations when there is severity of the symptoms.
Question 2
A female patient taking oral contraceptives should engage in discussion with the doctor. This is of relevance when the patient is taking antibiotics together with oral contraceptives (Coates, 2012). There is possible drug interaction between the contraceptives and antibiotics taken by the patients. In such cases, the patient should be forewarned of the impending dangers of getting pregnant. Caution needs to be taken in the dosing of oral contraceptives to avoid the associated side effects (Edmunds & Mayhew, 2013). The patient needs to understand that the low dosage of the contraceptives has a decreased efficacy when used concomitantly with the antibiotics.
Antibiotics interact with the oral contraceptives to result in low efficacy. Most birth control pills contain estrogen, and when used in combination with antibiotics, enzymes present in the liver contributes to the breakdown of the hormone. Some of the antibiotics kill the normal flora in the stomach which serves the primary role of activating the pills (Edmunds & Mayhew, 2013). Spotting is the first sign that indicates interaction of birth control pills and antibiotics. Examples of antibiotics that interact with oral contraceptives includes rifampin, sulfamethoxazole, ampicillin, minocycline among others.
Several considerations need to be put in place when discussing the issue of oral contraception and its interactions with antibiotics (Coates, 2012). In many societies, men become the primary decider of ways of having sex and may not recommend the use of alternative contraceptives such as condoms. Furthermore, personal values and beliefs can find an influence from the media and peer pressure. It is under the normal practice to give the patient information beforehand on the contraceptive choices for the best option (Coates, 2012).
Managing such drug interaction requires back up birth-control when antibiotics are administered at the same time. Backup methods of birth control have been recommended as ways of reducing the risk of getting pregnant while taking antibiotics (Anderson, 2012). Such approaches include abstinence, use of condoms or spermicide.
References
Anderson, R. J. (2012). Antibacterial agents: Chemistry, mode of action, mechanisms of resistance, and clinical applications. Chichester, West Sussex: John Wiley & Sons.
Coates, A. R. (2012). Antibiotic resistance. Heidelberg: Springer.
Edmunds, M. W., & Mayhew, M. S. (2013). Pharmacology for the primary care provider. St. Louis, Mo: Elsevier-Mosby.
1. Abstract
 Attributed to the increased antibiotic resistance, patients with severe infections receive treatment with less than the maximum treatments. The objective of the controlled consumption is to reduce the rise of antimicrobial resistance. The practice of controlling the consumption faces two dilemmas: either to benefit future patients whereas increasing the risks of present patients. More so, if the control process should be through disregard of the present patient’s autonomy. It is the sole role of doctors to safeguard the rights of the future patients. The most convenient way of maintaining a balanced scorecard between the two groups of patients require a collective decision-making process. A formal approach of protecting future patients by making a ratio of benefits to present patients and unidentified persons can aid in the regulatory measure of protecting the prevalence of the antibiotic resistance.
Attributed to the increased antibiotic resistance, patients with severe infections receive treatment with less than the maximum treatments. The objective of the controlled consumption is to reduce the rise of antimicrobial resistance. The practice of controlling the consumption faces two dilemmas: either to benefit future patients whereas increasing the risks of present patients. More so, if the control process should be through disregard of the present patient’s autonomy. It is the sole role of doctors to safeguard the rights of the future patients. The most convenient way of maintaining a balanced scorecard between the two groups of patients require a collective decision-making process. A formal approach of protecting future patients by making a ratio of benefits to present patients and unidentified persons can aid in the regulatory measure of protecting the prevalence of the antibiotic resistance.
2. Introduction
2.1. Overview of antibiotic resistance
Over the last century, antibiotics remain to be the answer to several bacterial infections facing patients. They are chemical substances secreted by living organisms. Particularly, doctors prescribe these drugs to cure diseases (World Health Organization, 2011). Most antibiotic treatments for both moderate and severe bacterial infections start empirically without the knowledge of the causing pathogen and its susceptibility to the antibiotic dosage prescribed. Unlike in the past, where antibiotics had high effectiveness while used on patients, currently, about two-thirds of patients prescribed with antibiotics, the workout of the dosage has negative outcomes whereas the treatment remains empirical during the entire treatment course (Finley, 2012). Decreased efficiency of antibiotics results from the resistance of the bacteria in the human body.
Antibiotic resistance, as presented in the argument above, refers to scenarios where antibiotics lose their ability to respond effectively to bacteria and other disease causing pathogens by either killing them or controlling them (MacGowan, 2013). In other words, it is the situations where bacteria become resistant to antibiotics. In these situations, despite the continued use of antibiotics, bacteria continue multiplying thus leading to the prevalence of the infection in patients. Bacteria resistance attributes to inappropriate empirical antibiotic treatment. Its impacts to patients is the increased mortality rate (Finley, 2012).
2.2. Causes of Antibiotic Resistance
Antibiotic resistance results from a couple of factors. One of the major cause of the resistance is drug abuse. Among many patients, they have a perception that whenever they are sick, the answer to their infection is antibiotic (Choffnes, 2010). Conversely, they present a continued cycle of antibiotic use. Apparently, according to pharmacology response on drugs, they articulate that the increased use of a certain drug (more precisely antibiotics), leads to reduced effect on the patient body. According to doctors, it leads to a resistance that equips pathogens with a mechanism of responding to the antibiotic thus avoiding its severe effects of them (Sköld, 2011).
In addition to drug abuse, improper use of antibiotics leads to antimicrobial resistance. In situations where pathologists prescribe drugs to patients presenting bacterial infections, severe symptoms fade away before completion of the dosage (World Health Organization, 2011). Normally, when patients feel an improvement of their condition due to the reduced symptoms, they often stop using the antibiotics. Nevertheless, the used drugs does not fully eliminate the pathogens level in the blood stream. It contributes to increase survival of bacteria due to the encounter with the inadequate encounter with the antibiotic and thus leading to their resistance to future similar antibiotic use on the patient (Finley, 2012).
In other situations, though not common, natural selection law, based on genetic mutation and passage of resistant genes from one bacterium to the other, leads to the accelerating antibiotic resistance. Genetic mutation refers to the rare but spontaneous change of the genetic makeup of the bacteria. According to a recent study on the cause of reduced effectiveness of penicillin on patients, it concluded that changes in bacteria genetic strides occur in one cell per million cells (World Health Organization, 2011). On the other hand, passage of resistant genes between pathogens as well contributes to the reduced antibiotic effectiveness. The most common method of acquiring the resistant genes from another bacterium is through conjugation. Apparently, the process entails passage of gene encoding resistance (Finley, 2012). Similarly, viruses pass resistance traits between bacteria. In their passage, resistant bacteria packages the resistance material on the head of the virus. The virus injects the material to other bacteria (Sköld, 2011).
2.3. Methods of resistance
Now, it is essential differentiating the reaction methods of bacteria defining their resistance to antibiotics. Some bacteria release enzymes that inactivate these drugs. When in the inactive form, thee pathogens push them out of these target cells to the blood stream where the patient excretes them. Additionally, some respond by eliminating the target cells. Often, antibiotics have designated target cells. Their actions to pathogens is maximum when in these cells. Nevertheless, when bacteria eliminate these cells, antibiotics lack their target cells leading to failure of eliminating the bacteria (MacGowan, 2013). Lastly, which presents the severe cases of bacteria; they block the entry points of the antibiotics. Interestingly, they have secretions that clog the entry points of the antibiotics thus eliminating their action in the cells. Surprisingly, some pathogens have an automatic pumping mechanism that act on the onset of the drug. The mechanism is responsible for pushing the antibiotic back before it reaches the target cells (Choffnes, 2010).
2.4. Thesis statement
In the modern society, despite the advanced technology and knowledge in different pathogens, the prevalence of the ethical dilemma is alarming. Contrarily, the dilemma is still raising concerns on scientists. Once a bacterium acquires the resistance mechanism of a certain antibiotic, it may as well have the ability of resisting the other antibiotics (Finley, 2012). Additionally, the bacterium may collect several resistance traits over time making it resistant to different families of antibiotics (Witte, 2013). Conversely, aimed at improving the overall effectiveness of these drugs, it is essential for doctors to have comprehensive knowledge on the future of antibiotics. There is a strong belief that on the factual approach that the future of antibiotics depends on research carried out on antibiotics action on pathogens (Sköld, 2011).
The paper has an objective of evaluating the future of antibiotics. The thesis of the paper states that, “the right of future patients to effective antibiotic treatment should be recognized and balanced against the right of present patients.”
3. Evaluation study
3.1. Data collection
The study aims at utilizing some already carried out research on antibiotic resistance. Similarly, the study will review several articles presenting related information on the future of patients using antibiotics based on the issues facing the present patients (MacGowan, 2013).
3.2. Results
The challenge of antimicrobial resistance is increasing globally. However, comparison of the prevalence of resistance in nations considerably differs depending on the use. Results on antimicrobial resistance indicated that European nations faced higher challenges in comparison with other nations. Apparently, as research by Centre for Disease Prevention and Control highlights that antibiotic resistance leads to increased suffering of patients, prolonged illness and in severe cases deaths. The study revealed that there are an approximate of 25 000 deaths annually in Europe resulting from resistant bacteria (Choffnes, 2010).
Observational studies reveals a comprehensive relationship between the use of antibiotics and the bacteria resistance. The study revealed that areas with high levels of antibiotic consumption have high levels of antibiotic resistance (Finley, 2012). Conversely, reduced consumption and reliance on these antimicrobial agents significantly leads to reduced levels of resistance. Randomized control of these traits reveals casual relationships in both levels (individual and community) (Sköld, 2011). A comparison between the rates of development of antimicrobial agents over the last half century reveals a drastic decline in the rate of development of antibiotics. Scientist study on presentation of antibiotic on patients revealed a variance in prescription based on the nature of the bacterial condition presented by the patient (MacGowan, 2013). Normally, in situations where antibiotics did not work on a patient, pharmacists always developed a new antimicrobial agent that would aid in controlling the infection (Coates, 2012).
In contrast, development of antibiotic in the modern society is declining. The declined rate attributes to failure of success in strategies of discovering new agents. Conversely, future patients will have a high dependence on strategies applied on the present strategies aimed at withstanding the challenge of bacterial resistance (Choffnes, 2010).
Despite the stipulated strategies controlling the rate of intake of these agents, study revealed an increase in antimicrobial agent reliance by 0.5 percent (Sköld, 2011). Additionally, increased sales of by 16 percent indicated an increased consumption of antibiotics. Study on patients using these agents stipulated that nowadays, patients often use these agents aiming at shortening and reliving severs symptoms presented by mild and respiratory tract infections (World Health Organization, 2011). In addition, approximately 84 percent of antimicrobial agents use were prescriptions by local practitioners. Surprisingly, approximately above half of the population had respiratory infections. More so, another study by Gjelstad projected that 60 percent of patients with bronchitis had antimicrobial agent prescriptions from the local practitioners (Drlica, 2011). It was the same case with 75 percent of patients with sinusitis. The study thus revealed that more than 33 percent of respiratory infections patients used antibiotics. In children, antibiotics aid in controlling acute otitis levels (MacGowan, 2013).
3.3. Analysis of the results
Antimicrobial agent use is a dilemma in nature. However, many arguments deny the fact it is not a dilemma. The first argument denying the dilemma is the claim that studies are aiming at covering pathogens while using these antibiotics (Choffnes, 2010). However, imperfect use of data is contributing to the variance on the outcomes from studies. Apparently, in cases with low percentage of resistant pathogens, practitioners do not use antibiotic agents that achieve 100 percent empirical results on many infections (Witte, 2013). Controlled use of these agents in these cases is due to the consideration of future resistance of the antibiotics (MacGowan, 2013). Based on the results from the studies, it is widely vivid that antimicrobial agent’s usage among patients is common in European nations and attributes to their accessibility to these patients. Over-counter cases reveal need for controlled access of these drugs. While doctors prescribe these antibiotics to their patients, they ought to make considerations on the possible future negative impacts of the continued use of these drugs (Coates, 2012).
If practitioners give maximum treatment considerations for the sake of the patients’ interests, that is preventing the side effects of the infections and preventing future infections by the pathogen, there is not ethical dilemma in the approach by the pharmacologist. However, future possible negative outcomes is less severe of patients undergoing empirical prescriptions in comparison to patients having inappropriate treatments (Witte, 2013). Formally, the cost of future resistance should not be the basis of inappropriate treatment with antibiotics. Therefore, based on the data revealed by the studies carried out, respiratory infections treatment with antimicrobial agents is an appropriate measure since its focus is mainly at curbing the prevailing symptoms in patients (Pandey, 2002). However, in other situations, described by improper diagnosis, where patients take antibiotics due to their perception of the prevailing symptoms, it is inappropriate for their actions. Often, they increases the formal possibility of future negative outcomes of pathogen resistance (Drlica, 2011).
Wide variations exists in the antimicrobial prescribing rates both at the individual and community level. Apparently, the most frequent prescription of antibiotics is three times. Normally, as presented in the study by Goossens, outpatient prescription is thrice higher in Europe nations as compared to other continent nations. These statistics reveal that a high number of patients prescribed with antibiotics barely enjoys substantial benefits from the consumption. Evidently, due to the large volumes of antibiotics of patients with respiratory-related infections who rely on antibiotics, the area makes a high contribution towards bacterial resistance. Conversely, primary health care has a priority of reducing the consumption rate in the area (Drlica, 2011).
It is unnecessary using antimicrobial agents in situations where they do not have any clinical benefit to the patient. However, at the individual level, it is unclear whether it is necessary using antibiotics for mild conditions (Choffnes, 2010). The decision of the best approach in such a scenario requires doctors to have balanced aspects. Similarly, it may lead to using the ethical principles. Beauchamp and Childress developed four ethical principles relevant during the decision-making before prescribing antibiotics to patients (Drlica, 2011).
Prior to making a prescription, some patients may demand a precise treatment. Doctors should respect the patient’s decision (autonomy) (Coates, 2012). Practitioners have the obligation of evaluating the relevance of the patient’s choice in the control of the bacterial infection. If the patient’s autonomy is appropriate, then the practitioner can prescribe the dosage. However, it is inappropriate (maleficent) for prescription of a potent drug that has potential side effects to the individual and the society (MacGowan, 2013). Thus, the evaluation should avoid harming the patient. Nevertheless, the patient’s autonomy may have some benefits in reducing the severity of the illness. In such situations, it is vital weighing out the justice of the benefits with the possibilities of increased risks of future side effects. Fair distribution of risks (side effects) and benefits on the patient is essential for future treatment using antibiotics (Sköld, 2011).
4. Discussion
When a practitioner prescribes antimicrobial agents to a patient, most likely, the drug has some necessarily important to the later. Mostly, practitioners have full satisfaction with their decision on the prescription if they are in line with the patient’s wishes and guidelines of the infection (Pandey, 2002). Apparently, though rare, some doctors prescribe using the patient’s autonomy overlooking the guideline advice. The decision mainly objects at increasing the patient’s satisfaction. However, satisfaction with the prescription decision does not imply the decision is appropriate (Sköld, 2011).
Several factors contribute to the physician’s prescription decisions. Insecurity with the patient, anxiety, patient’s pressure, fatigue and personal factors often contribute to some inappropriate decisions made by the practitioners on their patients. Apparently, basing an argument on the objectives of medicine (curing, relieving suffering and comforting patients), inappropriate prescription with antibiotics is a rational take focused on winning the patient’s trust and confidence (Choffnes, 2010).
Therefore, despite the knowledge of underlying future side effects from these antibiotics, they do not prevent practitioners from prescribing these agents on patients. Prescription of antibiotics based on non-pharmacological reasons contributes to the increased prevalence of antibiotic resistance (Coates, 2012). Driving force to these, reasons arise from patient’s personal factors and doctor’s uncertainty. Patient-related factors arise from their expectations from antibiotics and as well peer advice (Drlica, 2011). Apparently, while focused on eliminating these non-pharmacological factors, guideline advice should address both patient and prognostic issues.
The natural perception of the doctor is to treat fully the patient utilizing the available resources to the maximum. The main conflict while treating using antibiotics is the consideration of the welfare of the present patient and future patients. It is convincing that extreme continuous use of antibiotics will contribute to an increase in antimicrobial resistance. Thereby, it will significantly influence contribute to severe effects to the unidentified persons in the future using these drugs. Balancing of present patients’ rights of receiving maximum treatment and future patients’ rights is challenging to doctors (MacGowan, 2013).
Ethical justification of the relationships between these patients’ rights has a relation to the law of nature highlighting that both the present and future patients have equal right to health and preservation of life (Coates, 2012). Hence, balanced interests of these groups is vital. While safeguarding the rights of the future patients, doctors are the key role players. Fair distribution of healthcare resources between generations is the sole role of the doctors and present patients (Drlica, 2011). Accountability can enhance balanced rights between the two rights. If the antibiotic consumption increases and leads to massive side effects to the future generations, it is vividly clear that the doctor who made prescription to the past prior patient should be accountable for the outcome (MacGowan, 2013).
If the current society understands its role in safeguarding future patient’s rights, members will concurrently determine the best ethical models of balancing their rights with the future needs. The following are important measures that may contribute to balancing of rights.
i. Cost effectiveness
The approach sums benefits of several groups of people where it reaches a maximum aggregate result. Right balance attainment can be through temporal discounting measures by valuing the balanced benefits providing a high preference on far future over the near future patients (World Health Organization, 2011). However, the measure does not consider the patient’s autonomy. Among the Western nations, a patient’s decision is paramount (MacGowan, 2013). Thus, doctors accept the decision regardless the decision being detrimental to their health. However, as opposed to the cost effectiveness measure of balancing the needs between future and present patients, patient’s autonomy should be considerate of the future and undefined persons (MacGowan, 2013).
ii. Beauchamp and Childress (Four principles of bioethics)
These measures provide a positive link between future and the present patients by enhancing considerations in prescription decisions made (Drlica, 2011). The measure provides for a written guideline that aids in lessening the difficulty of examining the future and the present rights (Pandey, 2002). The bioethics principles define the patient-doctor encounter. In some situations, preference of increasing the present patient’s risks especially by a small amount aiming at reducing possible future risks on the future patient is essential. High reliance on the patient’s autonomy does not aid in the balancing the rights (Coates, 2012).
Concluding the discussion, the rights of future patients to maximum treatment using antibiotics should have a recognition and balanced against rights of present patients. To enhance fairness between these groups, decisions on antibiotic treatment should be collective. Despite the guideline of maintaining the patient’s autonomy, in some cases, waiving the decision in favor of the future rights is crucial to maintain balanced rights. Similarly, the prescribing personnel should have high levels accountability to safeguard the interests of future undefined persons (MacGowan, 2013).
5. Conclusion
In conclusion, patients with severe and moderate infections require treatment with controlled antibiotics. Doctors need to give these patients less than the maximum empirical antibiotics in response to increasing resistance. The practice involves ethical dilemmas. The dilemma of both delaying and controlling the consumption rates of patients in order to safeguard the future patients. On the other hand, the dilemma prevails on the decision of disregarding the patient’s autonomy. Collective decisions on antibiotic treatment is the convenient method of responding to the ethical dilemma facing pharmacologists. Cost-effectiveness discounts does not solve the challenge of balancing the future and the present rights. Antibiotic resistance is a social issue and poses a challenge to future patients. Therefore, present address of the issue is crucial in response to right s balance of patients.
Reference
Coates, A. R. M. (2012). Antibiotic resistance. Heidelberg: Springer.
Drlica, K., & Perlin, D. (2011). Antibiotic resistance: Understanding and responding to an emerging crisis. Upper Saddle River, N.J: FT Press.
Sköld, O., & Wiley InterScience (Online service). (2011). Antibiotics and antibiotic resistance. Hoboken, N.J: Wiley.
Choffnes, E. R., Relman, D. A., Mack, A., Institute of Medicine (U.S.)., Institute of Medicine (U.S.)., & National Academies Press (U.S.). (2010). Antibiotic resistance: Implications for global health and novel intervention strategies : workshop summary. Washington, D.C: National Academies Press.
Finley, R., & Solomon, M. (2012). Antibiotic resistance: Analysis & monitoring efforts. Hauppauge, N.Y: Nova Science.
MacGowan, A., Macnaughton, E., & Infections Part 1 of 3. (November 01, 2013). Antibiotic resistance. Medicine, 41, 11, 642-648.
Witte, W. (August 01, 2013). Antibiotic resistance. International Journal of Medical Microbiology, 303, 285-286.
MacGowan, A., & Macnaughton, E. (November 01, 2013). Antibiotic resistance. Medicine (united Kingdom), 41, 11, 642-648.
Pandey, L. (2002). Curb antimicrobial resistance: use the right antibiotic first!. (Brazilian journal of infectious diseases, 6, 5, 271-271.)
World Health Organization. (2011). Tackling antibiotic resistance from a food safety perspective in Europe. Copenhagen: World Health Organization.
What discussion should be had with the female patient taking oral contraceptives?
 The use of contraceptives has increased numerously over the past few years. When prescribing patients with contraceptives, it is important to engage them in a patient education regarding contraceptives. The physician should explain the various available methods of using contraceptives to the patient. For instance, contraceptives can be dosed using sterilization, use of oral contraceptives and also emergency contraceptives among other methods. In order to ensure that the patient avoids misusing the contraceptive, the physician should explain the effectiveness of contraceptive methods to the patient and also the risks involved (Lipsky & Ovid, 2011).
The use of contraceptives has increased numerously over the past few years. When prescribing patients with contraceptives, it is important to engage them in a patient education regarding contraceptives. The physician should explain the various available methods of using contraceptives to the patient. For instance, contraceptives can be dosed using sterilization, use of oral contraceptives and also emergency contraceptives among other methods. In order to ensure that the patient avoids misusing the contraceptive, the physician should explain the effectiveness of contraceptive methods to the patient and also the risks involved (Lipsky & Ovid, 2011).
What are the cultural considerations that should be made when having this discussion?
The use of contraceptives is a sensitive issue among many people. Thus, the contraceptive discussion between a patient and a physician should be handled with great professionalism. Some patients are limited to their beliefs, personal preferences and attitudes. Therefore, when talking to these patients, one should establish if there are any cultural considerations involved.
Great professionalism should be employed in this situation. This is because some patients may feel embarrassed or disrespected. One of the most vital contraceptive talks is the patients sexual life. The physician will at most times inquire whether the patient has any ongoing sexual problems or whether the patient wants a baby soon (Aronson, 2013).
What is the interaction between oral contraceptives and antibiotics?SubT
The interaction between oral contraceptives (OC) and antibiotics can lead to harm on the patient in various scenarios. According to studies, typical use of oral contraceptives with antibiotics such as penicillins and tetracyclines can lead to pregnancy on the user. However, this depends on the frequency of these oral contraceptives. When examining a small population of patients, oral antibiotics show no effect on various pharmacokinetics such as levonorgestrel, estradiol and norethindrone. Nevertheless, this is with the exception of rifampin (World Health Organization, 2012).
What steps should be taken in order to manage this drug interaction?
Women taking oral contraceptives should not use preparations below the required level of levonorgestrel and ethinylestradiol. However, a simple solution towards reducing the danger on oral contraceptives and antibiotics, the physician should consider alternative ways of contraception when dealing with patients currently prescribed antibiotics (Aronson, 2013).
References
Lipsky, M. S., & Ovid Technologies, Inc. (2011). Family medicine certification review. Philadelphia: Lippincott Williams & Wilkins.
Aronson, J. K. (2013). Meyler's side effects of endocrine and metabolic drugs. Amsterdam, NL: Elsevier.
World Health Organization. (2012). Medical eligibility criteria for contraceptive use. Geneva: Reproductive Health and Research, World Health Organization.
 Hormones are chemical messengers found in the body. Their transmission is through the bloodstream to the cells and tissues (Porth, 2009). Hormones influence different processes including growth and development, sexual functions, metabolism and as well mood. Release of hormones used in the body is because of the endocrine system that helps regulate and maintain different functions through the synthesis and release of hormones. Antidiuretic hormone (ADH) secreted in the posterior lobe of the pituitary plays a crucial role in the human body where it stimulates the reabsorption of water in the kidney (Norman, 1997).
Hormones are chemical messengers found in the body. Their transmission is through the bloodstream to the cells and tissues (Porth, 2009). Hormones influence different processes including growth and development, sexual functions, metabolism and as well mood. Release of hormones used in the body is because of the endocrine system that helps regulate and maintain different functions through the synthesis and release of hormones. Antidiuretic hormone (ADH) secreted in the posterior lobe of the pituitary plays a crucial role in the human body where it stimulates the reabsorption of water in the kidney (Norman, 1997).
This hormone is important in the human body since it conserves water. Its target organ is kidneys. Thyroid hormone (thyroxin) is another hormone secreted in the human body. Its secretion is in the thyroid glands and has its target cells as most of the body cells especially located in the skin. This hormone plays a role in stimulating metabolic rates essential for the normal growth of the body. Lastly, luteinizing hormone (LH) is another important hormone among females and males. Its secretion is in the anterior lobe of the pituitary and has its target being the gonads. It stimulates ovulation and as well the formation of the corpus luteum. In males, this hormone stimulates secretion of the hormone testosterone (Welch, 2011).
Receptor cells are cells located in the target cells. They control the secretion of these hormones. ADH, secreted in the kidney, has its receptors as hypothalamic osmoreceptors. They sense an increase in osmolarity that is capable of causing a disease. Other receptors linked with the hormone are atrial stretch receptors that sense change in central blood volume. Dysfunction of these receptors leads to diabetes insipidus. Receptor related to LH is luteinizing hormone- choriogonadotropin receptor (Norman, 1997). This receptor plays a great role in successful reproduction in human beings.
Its dysfunction in the body may lead to infertility, loss of menstrual cycles in female and as well loss of sexual drive. Lastly, hypothalamus and anterior pituitary are two receptors that control the secretion of thyroxine (Porth, 2009). These receptors control the levels of iodine in the body. Dysfunction may lead to hair loss, memory loss and as well muscle weakness. Severe cases may lead to coma and as well death.
Hyperthyroidism and hyperthyroidism are two conditions arising because of secretion of thyroid hormones. Hyperthyroidism arises due to over production of thyroid hormones than the body needs (Norman, 1997). On the other hand, hypothyroidism is a condition arising due to production of low quantities of thyroid hormones that are not enough for the body. Hyperthyroidism often results from a condition called Grave’s disease while hypothyroidism results from Hasimoto’s disease. Patients suffering from hypothyroidism often experience symptoms such as uncontrolled weight gain, increased sensitivity to cold, depression, excessive menstrual bleeding in females and lastly hoarse voice. On the other hand, hyperthyroidism patients experience symptoms such as increased sweating, muscle weakness, excessive weight loss, some irregular heartbeats and among female, they experience less frequent menstrual periods (Welch, 2011).
A blood test is among the most common test taken to differentiate between hyperthyroidism and hypothyroidism (Porth, 2009). During the blood test, doctors often check for the thyroid-stimulating hormone in the blood and as well, the free T4 and T3 hormone levels in the blood. Patients suffering from hyperthyroidism have high levels of T4 and T3 hormones. On the other hand, they have low levels of thyroid stimulating hormones. In contrast, patients with hypothyroidism have high levels of thyroid stimulating hormone and low levels of T3 and T4 hormones in their blood (Welch, 2011).
References
Porth, C.M., & Matfin, G. (2009). Pathophysiology: Concepts of altered health states. (Eight ed.) Philadelphia, PA
Norman, A. W., & Litwack, G. (1997). Hormones. San Diego: Academic Press.
Welch, C. (2011). Balance Your Hormones, Balance Your Life: Achieving Optimal Health and Wellness through Ayurveda, Chinese Medicine, and Western Science. New York: Da Capo Press.
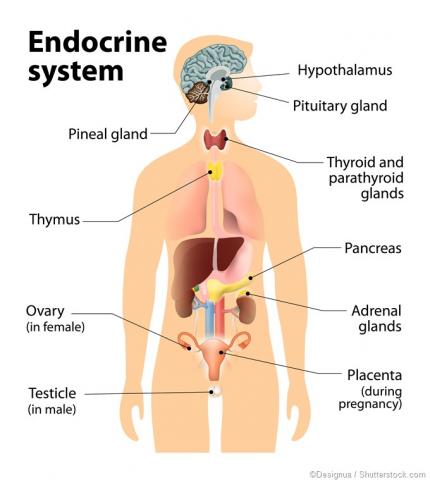 The endocrine system consists of chemical messengers, hormones, which are released into the bloodstream. Hormones control the internal body environment by regulating the body’s chemical composition. Further, hormones enable the body to respond towards environmental conditions that call for emergency demands. For instance, hormones respond to the following conditions; emotional stress, temperature extremes and dehydration. Hormones facilitate growth and development of body organs. Consequently, they regulate energy balance and organic metabolism (Porth, 2009).
The endocrine system consists of chemical messengers, hormones, which are released into the bloodstream. Hormones control the internal body environment by regulating the body’s chemical composition. Further, hormones enable the body to respond towards environmental conditions that call for emergency demands. For instance, hormones respond to the following conditions; emotional stress, temperature extremes and dehydration. Hormones facilitate growth and development of body organs. Consequently, they regulate energy balance and organic metabolism (Porth, 2009).
There are two groups of hormones namely the amino-acid hormones and steroid hormones. Steroid hormones function through messenger mechanism, whereas steroid hormones function through direct activation of genes.
The steroid hormone enhances stimulation of specific genes in the body through entering the target cells. Further, the thyroid hormone regulates metabolism in the body. The thyroid and steroid hormone are the two hormones that enter cells. The other hormones in the body do not enter cells. They simply function by binding with receptors on the surface of the cell, and they activate second-messengers in the targeted cells. For instance, the pancreas secretes insulin a hormone that regulates mineral and sugar balance in the body (Porth, 2011).
Hormones in the body have target cells. These target cells possess receptors that bind and transcript the hormonal message through receptors. Receptors are specifically modified to various target cells, and they only bind with specific hormones. Receptors only facilitate endocrine communication between the cell and the specific hormone. Different cells in various tissues in the body have different combinations of hormone receptors. The absence or presences of specific receptors determine the hormonal sensitivity of the cell (Porth, 2011).
Receptors in the cell are located inside the cell or in the cell membrane. Receptors for eicosanoids, peptide hormones and catecholamines are located at the cell membranes of the targeted cells. This is because the hormones are not lipid soluble. Therefore, the hormones bind with protein receptors on the exterior side of the cell membrane. These receptors are called extracellular receptors. On the other hand, intracellular receptors are located at the interior side of the cell membrane (Porth, 2011).
There are various diseases and disorders caused by hormonal dysfunction. Toxic adenomas, sebacute thyroiditis and pitituary gland malfunction are some of the hormonal disorders that may affect the endocrine system. Toxic adenomas develop when nodules grow on the thyroid gland and they start secreting excess thyroid hormones distracting body’s normal chemical balance. Further, subacute thyroiditis occurs when the thyroid gland leaks excess hormones due to inflammatory of the gland. On the other hand, pitituary gland malfunctions arise from hyperthyroidism (Porth, 2009).
Hypothyroidism is a condition resulting from reduced effect of the thyroid hormone on tissues. Hypothyroidism condition is either acquired or congenital depending on the site of abnormality. Hyperthyroidism condition exists where the thyroid gland overacts during hormonal reaction. The clinical manifestation of hypothyroidism depends on the age and severity of the disease. The major symptoms of hypothyroidism include fatigue, weight gain, cold intolerance and sleepiness. Hyperthyroidism patient symptoms include rapid heart rate, tremors, excessive sweating and enlarged thyroid gland (Porth, 2011).
Hypothyroidism can be directly measured in the blood by measuring the levels of thyroid hormone present in the blood. However, when the disease is mild or not fully developed the level of thyroid hormone in the blood may appear normal. Thus, the ideal way of testing hypothyroidism is by measuring the levels of thyroid stimulating hormone in the blood. A decrease in the blood TSH levels may lead to reduction of thyroid hormones secreted. While diagnosing hyperthyroidism, the blood test must indicate high levels of thyroid hormone present in the blood. However, the disorder may appear normal in blood test when it is in the primary stages. Thus, in this case hyperthyroidism is best measured through the thyroid stimulating hormones present in the blood. If the levels of TSH are high in the blood, then this portrays chances of hyperthyroidism (Zaidi, 2013).
References
Porth, C.M., & Matfin, G. (2009). Pathophysiology: Concepts of altered health states. (Eight ed.) Philadelphia, PA
Zaidi, S. (2013). Graves' disease and hyperthyroidism: What you must know before they zap your thyroid with radioactive iodine : a groundbreaking, revolutionary and comprehensive approach. Camarillo, Calif: iComet Press.
Porth, C., (2011). Essentials of pathophysiology: Concepts of altered health states. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
