+1(209) 348-9544
order@myessayservices.com
+1(209) 348-9544
order@myessayservices.com
![]() Are you in High School, College, Masters, Bachelors or PhD and need assistance with your essay or research paper? All you need is to buy a research paper written by a specialist in your academic field . When you buy a research paper from us, we offer you an original, nil plagiarized dedicated proofreader, writer and editors who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.
Are you in High School, College, Masters, Bachelors or PhD and need assistance with your essay or research paper? All you need is to buy a research paper written by a specialist in your academic field . When you buy a research paper from us, we offer you an original, nil plagiarized dedicated proofreader, writer and editors who is PhD or Masters qualified. MyEssayServices.com is an experienced service with over 9 years experience having delivered over 83,000 essays over the years.

What is Neurosonography?
 Neurosonography refers to a branch of medicine that is dedicated to taking of ultrasound scans on patients’ brains, as well as their nervous systems. This field is also referred to as neuroimaging or neurosonology. The primary motives of this highly specialized field are aimed at monitoring and diagnosing the flow of blood through the blood vessels of the patient located within the Central nervous System or the CNS as it is commonly referred to. Just like many other medical fields with sub-branches, neonatal Neurosonography is a sub-branch of this field. This branch specializes in the imaging of infants’ nervous systems. The open fontanelles of the neonate make it possible to fully analyze the neurological state of the neonate.
Neurosonography refers to a branch of medicine that is dedicated to taking of ultrasound scans on patients’ brains, as well as their nervous systems. This field is also referred to as neuroimaging or neurosonology. The primary motives of this highly specialized field are aimed at monitoring and diagnosing the flow of blood through the blood vessels of the patient located within the Central nervous System or the CNS as it is commonly referred to. Just like many other medical fields with sub-branches, neonatal Neurosonography is a sub-branch of this field. This branch specializes in the imaging of infants’ nervous systems. The open fontanelles of the neonate make it possible to fully analyze the neurological state of the neonate.
Many of the neonates subjected to this imaging are born either premature or preterm. This imaging is intended to investigate and determine the existence of any neurological disorders, or disorders of the nervous system. This field makes use of highly specialized equipment that is designed to image the brain of the neonate based on ultrasound technology to provide a detailed view of the neonate brain and nervous system. In this way, doctors are able to detect any abnormalities in the brain and nervous system. Neurosonography is also widely used in laminectomy procedures to assess the state of the spine.
Proper Instrumentation
Neurosonographic examinations are facilitated by the use of linear array transducers. These transducers can be either sector or curved. To generate images, these transducers emit an intense pulse of extremely high frequency into the tissue to be imaged. The arrival time and intensity of the acoustic echoes generated by the tissue enables the imaging of the tissue. The tissue acts as ‘reflectors’ hence enable imaging. The high frequencies used are responsible for developing high resolution images .
To assess the superficial structures such as the superior sagittal sinus, linear array transducers are the objects of choice. In cases where the anterior fontanelle has already fused, medics are forced to use low frequency transducers that have the ability of penetrating through the fused bone. In terms of instrumentation use, premature neonates demand the use of high frequencies while infants and full term neonates use lower frequencies. To ensure safety, Doppler power output of the instruments is regulated by the ALARA principle. This principle dictates that the Doppler power output should be As Low As Reasonably Achievable. In this way, instruments guarantee both safety and accurate high resolution results.
Guidelines
In order to regulate the practice of Neurosonography, and facilitate safe and accurate procedures, AIUM (American Institute of Ultrasound in Medicine) has put in place guidelines that all practitioners must follow. The first and most vital is that Neurosonography shall be performed on infants only in the existence of valid medical reasons. This goes on to add that the lowest possible ultrasonic exposure setting is to be used during the procedure .
The guidelines assert that Neurosonography in term and pre-term neonates is used for reasons such as to assess for hydrocephalous, presence of congenital malfunctions, to screen for parenchymal abnormalities and hemorrhage in pre-term neonates, to determine the presence of hypoxic ischemic encephalopathy and as follow-ups on previously documented problems.
However, AIUM understands that restricting medics to these golden rules can in itself be harmful. The variant nature of abnormalities and conditions make it virtually impossible to treat one patient like the other. In such cases where additional information is a prerequisite of the diagnosis and healing process, practitioners are allowed not to break, but instead to circumvent these rules in pursuit of medical explanations. Although such procedures are incapable of detecting every possible abnormality, they prove to be highly effective in detecting most of them. It is for this sole reason that AIUM permits the ‘skirting’ of the law insofar as Neurosonography guidelines are concerned.
Standard Protocols
The need to provide quality ultrasound services demands the use of standard protocols to dictate the operation of the industry. In order to perform diagnostic medical ultrasounds, all individuals are required to be medical practitioners that are accredited and reviewed by AIUM. In this way, quality is guaranteed in terms of conducting the procedure, as well as interpretation of the results. All physicians are required to hold a valid state license and to undergo re-accreditation procedures by AIUM every three years. The need to remain afloat in the rapidly evolving world of medical technology demands that all physicians involved in conducting and interpreting ultrasounds are retrained in terms of use of new machinery and techniques.
Sonographers are required to be certified in their specialties, and must remain so in order to achieve AIUM accreditation. Sonographs are given a time limit of two business days to be read and their findings given to the patient. Mechanisms are also in store to ensure that patients are contacted as soon as results are released and that emergency findings can be addressed immediately while paying attention to patient safety. Seeing that it is a branch of medicine, medical ethics laws apply to sonographers, as well. Maintaining doctor-patient confidentiality, filing of reports, prevention of infectious diseases and the application of the ALARA principle all rank highly in the ethics codes on the practice of Neurosonography.
Normal Anatomy of the Neonatal Brain
A normal neonate that was carried to term has fully developed neonatal features. The cortical folding of the brain of a normal neonate is similar to that of an adult. The folds are fully developed, and all the sulci have already been formed by the time of birth. In healthy neonates, small remnants of the germinal matrix can be seen in the caudothalamic notch. They can also be spotted on the posterior end of the thalami, almost at the junction formed together with the optic radiation.
Myelination of the ventro-lateral nucleus of the thalamus (VLNT), the globus pallidus (GP) and the brain stem is evident at birth, as well. Unmyelinated white matter can also be seen in the hemispheres. The corpus callosum is also unmyelinated in a healthy neonate carried to term. At birth, the thalami and basal ganglia of a normal neonate are large and outrightly divided by the internal capsule. The brain stem of a healthy neonate is also well articulated. The decussation of the superior cerebellar peduncles, the quadrigeminal plate, the medial lemnisci and medial longitudinal fascicule are all clearly seen. The developmental stages in which many of these parts are in at birth form the basis of determining whether the child is normal or abnormal.
Abnormalities in the Neonatal Brain
Acquired
These are abnormalities that neonates acquire after their birth. The causes may vary from injury to infection of the neonate, but they are not passed down through parent-child relationship via birth or genetic inheritance (6). The fragile state of the neonate exposes it to an array of dangers, seeing that one can easily inflict injury upon it. Such injury can expose the neonate to diseases such as lymphoblastic leukemia, cardiomyopathy and myocarditis. These diseases can also be influenced by the environment in which the neonate is placed. The presence of pathogens that are capable of infecting the neonate with diseases plays a central role these diseases. However, Neurosonography can also be used to detect such diseases in neonates.
Congenital
There are also a number of diseases that many people inherit genetically from their parents. Neonates are no exception to this rule, seeing that they too are sufferers of abnormalities such as congenital heart disease and asphyxia among other diseases. Unlike the acquired abnormalities, these are purely genetic and are passed down from parents to children. Neonates particularly suffer a lot from this disadvantage.
Most Frequent Pathologies
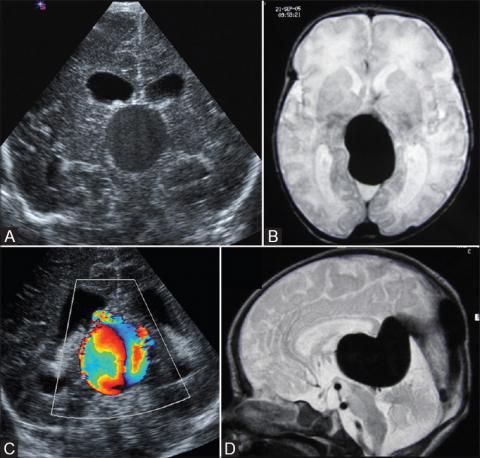
Neonates are fragile in nature, and many of them have been known to suffer from different kinds of pathologies. One of the most common and fatal pathologies is hydrocephalus (4). This refers to the enlargement of the ventricular system and is a very painful experience for the neonate. It can be either obstructive or communicating hydrocephalus. Another pathology common in neonates is hemorrhagic. This refers to subependymal intraventricular bleeding. As a form of pathology, it is most common in pre-term neonates (1). Such neonates weigh in at less than 1500 grams birth weight and are less than 32 weeks.
The caudothalamic groove proves to be the most common location. This pathology is classified into four categories, Grades I, II, III and IV. Periventricular leukomalacia is another common pathology. It is characterized by the necrosis of the white matter usually near the lateral ventricles. Being an ischemic lesion, it is the most frequent one on the immature brains of neonates. It can be diagnosed as either acute or chronic.
Another form of pathology is holoprosencephaly. This pathology is the result of a disturbed ventral induction process in the early stages of development in which the brain fails to form bilateral cerebral hemispheres (4). Agenesis of the Corpus Callosum is also a common pathology. It can refer to either the presence of narrow frontal horns coupled with an absent CSP, or the absence of the Corpus Callosum.
Applications of Neurosonography
In the Ultrasound Room
In the ultrasound room, Neurosonography has a number of applications. First and foremost, it can be used to determine the presence of neurological abnormalities in neonates (2). The use of this approach in scanning the brains of the infants is able to indicate any brain abnormalities. Though it may fail to expose every abnormality, it succeeds in exposing a large number of them. Secondly, the use of sonographs to determine the locations of tumors in laminectomy procedures to assess any abnormalities in the spines is another fort relying on Neurosonography.
In the OR
The Operating Room (OR) has its fair share of uses for Neurosonography. In Turkey, for instance, three dimensional Neurosonography has been used to treat tumors located along the spine. Through the use of Neurosonography, the doctors were able to map out the location and position of the tumor, and proceed to successfully remove it (4). The use of intra-operative 3D Neurosonography has been used to remove 6 intra-medullary and 22 extra-medullary tumors from patients in Turkey. The possibilities of this method becoming the standard measure insofar as neurological surgery is concerned only serve to raise the profile of Neurosonography.
References
Edwards, M. K., Brown, D. L., Muller, J., Grossman, C. B., & Chua, G. T. (1981). Cribside neurosonography: real-time sonography for intracranial investigation of the neonate. American Journal of Roentgenology, 136(2), 271-275.
Fischer, A. Q. (1985). Pediatric neurosonography: Clinical, tomographic, and neuropathologic correlates.New York: Wiley.
Girard, N., Gire, C., Sigaudy, S., Porcu, G., d'Ercole, C., Figarella-Branger, D., ... & Confort- Gouny, S. (2003). MR imaging of acquired fetal brain disorders. Child's Nervous System, 19(7-8), 490-500.
Graziani, L. J., Mitchell, D. G., Kornhauser, M., Pidcock, F. S., Merton, D. A., Stanley, C., & McKee, L. (1992). Neurodevelopment of preterm infants: neonatal neurosonographic and serum bilirubin studies. Pediatrics, 89(2), 229-234.
LaRusso, S., Goss, S. E., Jackson, M. L., & Society of Diagnostic Medical Sonographers (U.S.). (2009). NCER National Certification Exam Review: Neurosonography. Plano, Tex:Society of Diagnostic Medical Sonography.
Proctor, M. R., & Black, P. M. L. (2005). Minimally invasive neurosurgery. Totowa, N.J: Humana Press.
Introduction
 Medical imaging is technological advancement in the modern medicine used to view the internal body organs. Medical imaging has brought a new dimension in the medical scene by giving precise view of the body especially during sensitive surgeries (Bankman 67-77). In the case of broken bones or internally injured organs, medical imaging aids in the correction of the problem that would be difficult through conventional means. Ionizing radiation has found the high application in hospitals and clinics for performing the diagnostic imaging. In this application, the common forms of radiation used are x-rays and gamma rays (Bankman 67-77). Medical imaging is appropriate for accurate diagnosis of diseases and injuries. They provide the requisite information to the doctor, which goes a long way in reciprocating appropriate care. Specialist trained for administering these procedures need to use the least amount of radiation. Despite the dictated use of a small amount of radiation, there still exist potential risks especially when there is over exposure and neglect. The risk is to the patient and the technologist in the same context.
Medical imaging is technological advancement in the modern medicine used to view the internal body organs. Medical imaging has brought a new dimension in the medical scene by giving precise view of the body especially during sensitive surgeries (Bankman 67-77). In the case of broken bones or internally injured organs, medical imaging aids in the correction of the problem that would be difficult through conventional means. Ionizing radiation has found the high application in hospitals and clinics for performing the diagnostic imaging. In this application, the common forms of radiation used are x-rays and gamma rays (Bankman 67-77). Medical imaging is appropriate for accurate diagnosis of diseases and injuries. They provide the requisite information to the doctor, which goes a long way in reciprocating appropriate care. Specialist trained for administering these procedures need to use the least amount of radiation. Despite the dictated use of a small amount of radiation, there still exist potential risks especially when there is over exposure and neglect. The risk is to the patient and the technologist in the same context.
This paper explains in detail the potential risk associated with exposure to these forms of radiation. Some forms of radiation include x-rays and high penetrating gamma rays. X-rays are performed with the help of an x-ray machine and another sophisticated CT or CAT scan machine. The paper employs the why methodology in researching on the topic. There are a total of five whys in the whole paper with each forming a standalone point. An account on the disadvantages of excessive radiation exposure is provided.
The second part the paper tries to explain the risks associated with over-exposure. Most hospitals often produce radiation wastes in the imaging process (Dössel 56-66). The paper will expound on the adverse environmental consequences. As a control measure, the paper will explain the importance of reducing the over reliance on medical imaging or rather further reduction of the dosage. Some of the risks associated with over exposure to the radiation are explained and can only be reduced through good training of the technologists. The quality of each why is crucial to the whole research practice. Thesis statement: Medical imaging contributes to trace amounts of radiation in the body that have adverse effects to the system of patients exposed.
Why excessive Radiation is bad?
Gamma rays and X-rays are in common use, in medicine. X-rays pass through the body forming a picture on film or a computer/television monitor. The interpretation of the image can be done by a radiologist. X-ray machine or CAT or CT scan machine are commonly used in imaging. Nuclear medicine is the latest technology in which small amount of radioactive material is either inhaled or swallowed by the patient. The radioactive material emits certain quantum of energy. The radiation emitted by the radionuclide helps in visualizing the internal organs or damaged tissues. In the normal procedures, the radionuclide disappears from the body within hours after administration (Suetens 78-82).
Typical values of x-ray dosage have been stipulated for the application in medicine. The dosage may differ from one person to the next due to the differences in the machines used and the metabolic status. Background radiation from the standard unit for measuring the diagnostic x-ray and nuclear medicine exams. Gamma rays are emitted by radionuclides injected or administered in the body. These rays are high in energy and are associated with damaging effects on the body genetic make-up.
Gamma rays and X-rays are ionizing radiation since they are capable of displacing an electron from its orbit. The effect of this phenomenon on the DNA molecule can either be direct or indirect. Indirect when the electron hits a DNA strand causing the damage or Indirect when the electron reacts with the water molecule creating a powerful radical the can damage the cell’s DNA. This has dire consequences since DNA damages may induce malignancy. Other effects are evident depends on radio sensitivity that occur mainly in mitotic or undifferentiated cells. Some organs are, therefore, more radio sensitive than the others and this contributes to potential risks as well as damages.
The use of ionizing radiation in imaging is on the rise due to the accuracy in revealing the body’s internal organs and tissues. Ionizing radiation is commonly used and comprise of a high-energy wavelength. The potential risks from ionizing radiation are the damage to the DNA, though the cells have the inherent machinery of repairing these damages. In some cases, the repair is imperfect thus, leaving behind distorted DNA sequence (Suetens 78-82). Accumulation of such repairing mistakes contributes to rising cases of mutations. Higher dosage of radiation arises from nuclear imaging and CT scan which require larger significant amounts of radiation, unlike the traditional x-ray imaging. A CT scan of the chest requires 10 times more radiation than the normal chest x-ray imaging. Excessive radiation that affect the germ line such as testes and ovaries may influence some hereditary disease or abnormalities that can be passed to the coming generation. Such risks necessitate extra caution such as placement of lead rubber shields covering the gonads.
Why the delays/ mistakes/ over-exposure increases the risks?
Diagnostic medical imaging contribute to a possible increase in the risk and exposure time. Though most of the errors are perceptual or interpretive in nature, procedural errors are common. Some of the risks include overdosing the patient in case of radionuclides or overexposure in case of x-ray or CT scan. Some errors in medical imaging arise from ignorance or neglect by the medical officer carrying out the test. Plain radiography and Computed Tomography contribute to frequent imaging errors. In plain radiography, X-ray imaging contributes to a high percentage of error in imaging. The CT scan errors are common and may contribute to gastrointestinal tumors. Diagnostic errors have been reported in many quarters where medical imaging is performed. Approximately 31 percent of radiologist have faced a claim in their career.
There are common suits with regards to the procedural complication and the radiologist-referrer communications. Other concerns the failure to recommend additional testing. The main interest in these errors is the potential risks posed by the lengthy exposure. The more the exposure to the ionizing radiation the high the risks increase to general health-related issues. The risk increases when there is overexposure to the radiation. Errors relating to overdose with radionuclide means that the body will have low clearance rates. This will increase the accumulation of residual radioactive chemicals in the bones, teeth and other vital organs. This will lead to release of radiation that may cause extensive damage to the DNA. This culminates into possible incidences of cancer.
Nuclear medicine and other imaging methods provide information both at the molecular and cellular level thus contributing to the determination of the health status of the patient (Metaxas 76-81). They entail measuring the uptake and the turn-over of specific radio-tracers in the organs. The main process functional to nuclear imaging include cell-cell interactions, trafficking and homing, programmed cell death (apoptosis) and neurotransmitter activities.
Medical imaging offers the newest way of probing the healthy and diseased states of the tissue and their response to treatment. The similarity in all of these processes is that they take a specific timing. The technologist must, therefore, administer the right doses of radio-tracers and exposure to the rays used in the imaging. Failure to these practices will contribute to devastating effects of over-exposure to the rays. The risk associated with continued exposure to these rays leads to extreme cell damages. Most of the procedures are, therefore, performed under specified period of time. Errors arising from wrong timing and long exposure contributes to poor results and further exposes the patient and the technologist to the damaging effects of radiation.
Carcinogenicity arising from high extreme of radiation contributes to the Warburg Effect, a situation where tumor cells consume large amounts of glucose than the normal cells (Suetens 78-82). Over-exposure to radiation due to poor timing contributes to the adverse effects to the integrity of the cells and the tissue. The potential risk associated with the exposure include damaging the cell’s DNA and the cell signaling process. Most of the medical imaging procedures are made with considerable caution and hence regarded safe. Human is to error and these may go undetected. A common scenario can be poor imaging requiring a repeat of the procedure (Suetens 78-82). A repetition of the procedure increases the exposure levels of the patient to harmful radiation. This trickles down to further cell damage at molecular level. Incidences of malignancy and cell death attributable to over-exposure to radiation increases in the body system. It is mandatory for the radiologist to adhere to the procedure in carrying out medical imaging to avert unnecessary health outcomes.
Why radiation waste is harmful?
Medical imaging results in the production of significant amounts of radioactive waste. Despite the measures put in place to prevent escape of radiation from the hospitals, small burst is released to the immediate surroundings. The greatest concern of these releases is the effect they may have on the biodiversity as well as the non-targeted group of people. Radionuclide waste from the medical institution has high environmental effects when they come in contact with living organisms in these sites. The same cell damaging effects of radiation on man are extended to other organisms. The waste comprises of low doses of ionizing radiation (Metaxas 76-81). Specific attention is paid to the radio sensitivity in the organism that comes into contact, as well as cancer and non-cancer effects of these radiations. Environmental Health and Safety conducts extensive research on the optimization of medical doses in radiology, nuclear medicine and other radiation therapies. Effectiveness of radiopharmaceuticals and their degradability in the environment should be a major consideration before they become full blown environmental results (Broder 48-52).
Poor management in radionuclide waste and potential release to the environment has dire consequences on the living organism in the biosphere. Radionuclide behavior especially in degradability has induced effects in the non-human biota. There are atmospheric, aquatic and terrestrial dispersion of these wastes with most of them finding their way into these systems through the food chain (Suetens 78-82). Most of these wastes have a half-life of one to several days and depending on the metabolism of the organisms, the degradability may vary.
Residual effects may last for long periods especially for organisms that are used for human consumption such as fish. Cell damage from high penetrating power gamma rays produced by the radionuclides contributes to high mutation rates in these organisms. Long-term management of radioactive waste from medical imaging procedures will safeguard the lives of organisms and other human beings. It is appropriate for the hospital management and staff to ensure safe decontamination and segregation of waste in biohazard kits. Negligence is the prime factor contributing to the release of medical imaging waste to the environment (Broder 48-52). In this unethical practice, hospitals and other medical centers mix radionuclide waste with other clinical waste. Accountability and sound waste management programs will help in protecting the environment and the flora and fauna.
Why reduction in excessive medical imaging is good?
Hospitals and other health experts should drift from over reliance on nuclear imaging and exposure to x-rays. Medical imaging is a great technology providing real-time results on diagnosis of the medical situation. Despite the accrued benefits from these novel procedures, reducing excessive medical imaging will have advantages in the decline in incidences of adverse effects to the patients. Programs should be put in place in medical centers to prevent subsequent exposure of the same patient to radiation. In this context, the patient who has been exposed to CT scan in a previous medical diagnosis should not be recommended to the same procedure. This brings in the advantage of keeping data relating to patient. Understanding the clinical history of the patient will reduce the use of excessive medical imaging. Alternatives can be sought such as Magnetic Resonance Imaging in preventing excessive exposure to the ionizing radiation. The benefits of moving away from excessive medical imaging entail poor releases of radionuclides to the environment and thus an overall reduction in waste.
Through the realization of adverse health effects resulting from ionization radiation, many hospitals and health care centers have opted for safer imaging procedures. An example of such procedure is the se of ultrasound (Bankman 67-77). The technique r educe the complication rates when compared to the use of ionizing radiation for imaging. In increasing diagnostic accuracy, Ultrasound has found application in focused assessment with sonographer for trauma, a test administered for signs of internal bleeding. The procedure does not lead to high exposer rate to ionizing radiation and it is the preferred choice for diagnosing children, as well as medical analysis for kidney stones. MRI is regarded as an alternative to ionizing radiation in patients. Children and young adults have a high specificity to radiation exposure. Informed consent helps the patient to maintain autonomy in deciding the course of his/her health care (Bayliss, and Langley 45-49).
Medical imaging using ionizing radiation can find other alternatives especially in the situations when the patient had a previous exposure. Alternative to ionizing radiation include those that have a lower dosage. CT scan requires high doses of radiation in comparison to plain X-rays, mammography and fluoroscopy. It is necessary for the patient to seek guidance in making a choice for the appropriate imaging technique (Broder 48-52). In the PET (Positron Emission Tomography), a procedure used in nuclear medicine make use of short-lived pharmaceuticals for specialized diagnostic tests e.g. cancer and epilepsy. This can be an alternative to other imaging techniques in nuclear medicine that use radionuclides with a longer half-life. To zero-rate on the dependence in ionizing radiation for imaging, MRI scans and Ultrasound are appropriate.
Why training in medical imaging will avert some of the potential effects to the system?
Nuclear medicine has many benefits and thus, cannot be ruled out in medical practice. Solving issues relating to over exposure would require high specialty (Bryan 88-93). Training should be done to the radiologist to prevent the common mistakes associated with the practice. Diagnostic radiology provides images of high quality that helps in understanding the medical problem or symptom. These techniques are fast, accurate and non-invasive. All these techniques have set procedures that should be adhered to in diagnosis (Dössel 56-66). Mistakes by the radiologist as previously stated may lead to overexposure to overdose in the case of radionuclide. This has adverse effects on the patient exposed to the radiation and keeps the integrity of the practitioner into question. Nuclear medicine specialist and radiologist should ask the patients on whether there was previous exposure to the same radiations (Bryan 88-93). Other recommended imaging practices may be sought after.
Well trained specialist will avert potential delays and mistakes in administering the procedures. Radiologists and nuclear medicine experts should have the knowledge on the electromagnetic waves, operation of the machines, and good dexterity in the measurement of the radionuclides, and good command of interpretive skills. All these factors lead to the overall prevention of errors arising from negligence (Carver, and Carver 68-75). Ethical qualities of the specialists should be a strong factor in the whole field. Errors in nuclear imaging arise from negligence but not lack of knowledge. Procedural practices in administering radionuclides and helping the patient with informed consent are some of the ways that will bring professionalism in the whole field. Specialist should be aware of environmental management system and thus dispose of radionuclide waste in the correct manner. This will entail placement of this waste in the correct kits labelled with a biohazard sign.
Why and how do patients get excessive imaging studies in the hospital?
Increase in medical imaging using ionizing radiation is further attributed to in-existence of a communication platform between the doctor and the patient. Before administering of such procedure, it would be appropriate for the doctor to know the history of his/her patient. Alternative procedures can be applied in instances when the history indicates previous exposure of the radiation to the patient (Bayliss, and Langley 45-49). It also under a huge assumption that medical imaging is the best practice available for checking the internal status of the body. The “best practice doctrine” has led to overindulgence into the procedure thus increasing the exposure levels to radiation. Another factor contributing to overexposure to radiation concerns the referral hospitals that are owned by the learning institutions. Medical imaging may be done on high frequency as a teaching mode to the medical students.
Economic effects are some of the reasons behind increased medical imaging. Most hospitalization cases get reimbursements through the DRG format (Dössel 56-66). The imaging services offered are non-reimbursable. These services, therefore, drain the hospital finances in the long run. Most medical operations fall under the same class as insurance and payment operations and, therefore, these scans would be discouraged. Exposure to radiation is on the rise because medical imaging is done at “fee-for-service” in many clinics. This is because they are income generating compared to other diagnostic procedures. The medical imaging rates and radiation exposure has been on the rise because of a change in the general fee structure of radiological exams and capping reimbursements.
Conclusion
Medical imaging and services during hospitalization and the excessive exposure leads to adverse effects on the patients. These effects relate to over-exposure thus, increasing the risks and potential dangers in to the health status. The whys in the investigation of this problem gives an explanation ranging from the effects on the patient and the adverse effects extrapolating to the environment. Forms of radiation and their effect on the body include the gamma rays, x-rays and destruction of the DNA which affects the integrity of the cell.
These contribute to advancement towards malignancy and cancerous tumors. It is important for the doctor to do a consultation with the patient before conducting any of the diagnostic imaging. Overexposure to ionizing radiation can be contributed by an increased error rate of the nuclear specialists (Dössel 56-66). Training of these specialists will help in averting these cases of overexposure and, therefore, result in a total reduction, in health associated dangers (Carver, and Carver 68-75). Medical Imaging services should not be scrapped off but rather be controlled to prevent rising cases of the after effects of continued exposure (Suetens 78-82).
References
Bankman, I N. Handbook of Medical Image Processing and Analysis. Amsterdam: Elsevier/Academic Press, 2009. Print.
Bayliss, C R, and K F. Langley. Nuclear Decommissioning, Waste Management, and Environmental Site Remediation. Amsterdam: Butterworth-Heinemann, 2003. Print.
Broder, Joshua. Diagnostic Imaging for the Emergency Physician. Philadelphia, PA: Elsevier/Saunders, 2011. Print.
Bryan, R N. Introduction to the Science of Medical Imaging. Cambridge: Cambridge University Press, 2010. Print.
Carver, Barry, and Elizabeth Carver. Medical Imaging: Techniques, Reflection and Evaluation. Edinburgh: Elsevier, 2012. Print.
Dössel, Olaf. World Congress on Medical Physics and Biomedical Engineering: 7-12 September, 2009, Munich, Germany : Radiation Protection and Dosimetry, Biological Effects of Radiation. Berlin?: Springer, 2009. Print.
Metaxas, Dimitris N. Medical Image Computing and Computer-Assisted Intervention - Miccai 2008: 11th International Conference, New York, Ny, Usa, September 6-10, 2008 ; Proceedings. Berlin: Springer, 2008. Print.
Suetens, Paul. Fundamentals of Medical Imaging. Cambridge, UK: Cambridge University Press, 2002. Print.
Browse More Essay Topics 24/7/365 Support 11+ Yrs in Essay Writing Pay for Quality not Quantity Score that A+ Grade
Affordable Papers
Research Paper for Sale
Cheap Research Papers
Buy Term Papers
Buy Research Paper
Write My Paper
Buy an Essay
Cheap Essay Writer
Write my Essay
Thesis Help
Dissertation Help
Paper Writing Service
Pay for Homework
Pay for Research Paper
Do My Essay for Me
Pay for Essay
College Papers for Sale
Do My Homework for Me
College Essays for Sale
Buy Research Papers Online
Buy College paper
Client: "(Berlin, G.K., CA)"
Topic title:"Leadership shortfalls in Blue Chips"
Discipline: "Economics"
Pages: 5, (APA)
" Awesome, the writer delivered it as required by the professor. They also sent me a plagiarism & grammar report Wow!. I was worried about how the essay would turn up but this is exactly what wanted. Thank you and will be back with a longer essay"
Accounting Research Papers
Business Research Papers
Communication Research Papers
Computer Science Research Papers
Economic Research Papers
Film Studies Research Papers
Finance Research Papers
Geography Research Papers
History Essays
Psychology Research Papers
Political Science Research Papers
Nursing Research Papers
Mathematics Essays
Management Essays
Literature Essays
Law Essays
World Affairs Essays
Technology Essays
Sociology Essays
Science Essays
Religion Essays
+1(209) 348-9544
Terms
Privacy
Sitemap
Frequently Asked Questions
0% Plagiarism Guarantee
Money Back Guarantee
Revision Policy
